3 Fetal Alcohol Spectrum Disorder
Katie Massie
History & Introduction
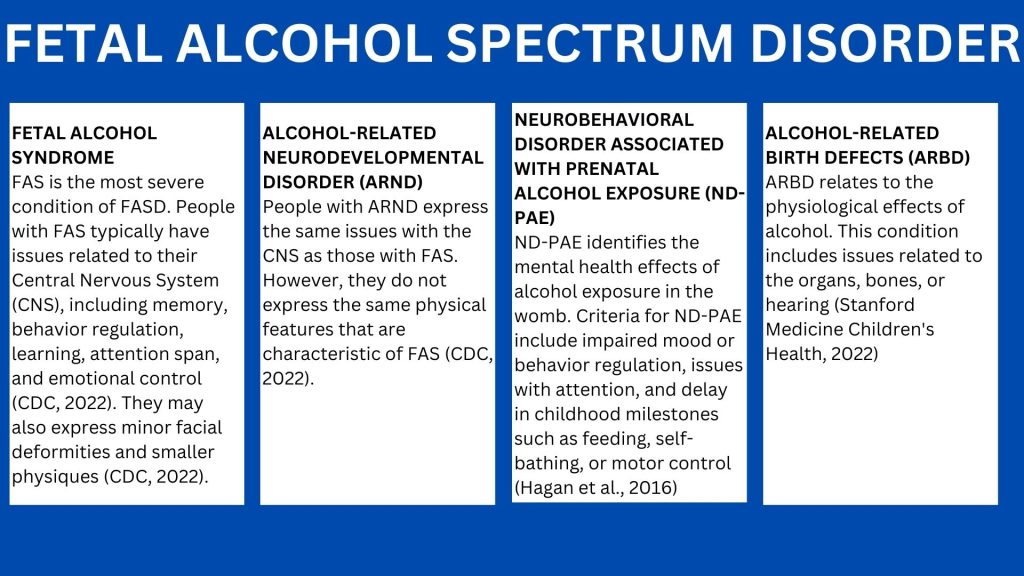
For as long as alcohol has been consumed, Fetal Alcohol Spectrum Disorder (FASD) has existed. In the 1800s, Charles Darwin’s Origin of the Species introduced the idea of genetics and inherited disorders to the general population (Brown et al., 2019). As a result, the impacts of alcohol on development caught the public’s attention. In the 1950s, birth defects caused by the thalidomide tragedy amplified this concern about environmental-related effects on fetal development (Brown et al., 2019). Despite the prevalence of alcohol in American history, it was not until 1973 that a team of American dysmorphologists, Kenneth Jones and David Swift, published their findings on alcohol and pregnancy, coining the term Fetal Alcohol Syndrome (FAS) (Armstrong, 1998). Coinciding with the rise in awareness of child abuse and battered child syndrome in the 1960s, physicians deemed FAS a tragic disorder and moral issue, igniting a wave of concern about maternal behaviors and childhood trauma (Armstrong and Abel, 2000). Today, FAS falls under the broader diagnosis of Fetal Alcohol Spectrum Disorder (FASD), which also includes Alcohol-Related Neurodevelopmental Disorder, Alcohol-Related Birth Defects, and Neurobehavioral Disorder associated with prenatal alcohol exposure.
What is Fetal Alcohol Spectrum Disorder?
FASD is a collection of conditions caused by alcohol exposure during pregnancy. The effects of this condition include, but are not limited to, cognitive or behavioral issues, abnormal facial features, and growth stunts ranging from minor to severe (Wilkoit et al., 2017). Today, experts approximate that FASD affects as many as 1 to 5 out of 100 American children (CDC, 2022).
How does alcohol affect fetal development?
Alcohol is a teratogen. The structure of alcohol allows it to pass through the placenta and accumulate in the amniotic fluid (Jacobsen et al., 2022). Studies show that alcohol can damage brain cells, particularly in the hippocampus and amygdala (Jacobsen et al., 2022), resulting in slowed cognitive abilities. Alcohol can also damage the genes of a fetus, particularly those that impact physical feature development (Jacobsen et al., 2022). Because the size of the fetus is very small, weighing less than half an ounce, the effects of alcohol are much more significant than an adult’s. Opioids can also harm the developing fetus during pregnancy and lead to neonatal opioid withdrawal syndrome.
Signs and Symptoms
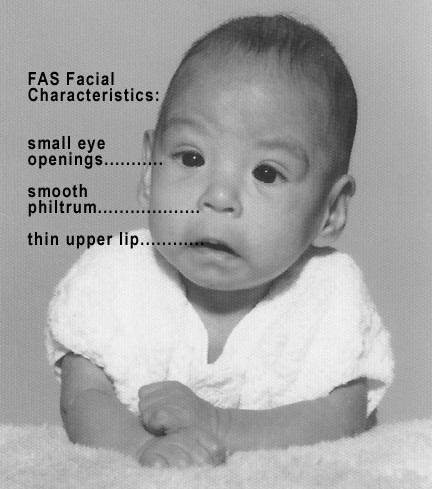
The symptoms of FASD range in severity and differ between individuals. To be diagnosed with FASD, a child must have issues surrounding growth, brain damage resulting in cognitive and behavioral delays, abnormal facial features, and alcohol exposure in the womb (Wilkoit et al., 2017). Physical abnormalities include a small head size, thin upper lip, low body weight, and below-average height (CDC, 2022). Symptoms regarding cognitive or behavioral delays include hyperactive behavior, poor control over body movement, low IQ, problems with speech and language, and poor judgment (CDC, 2022). The image below illustrates the facial characteristics of a child born with FAS.
Risk factors
While FASD affects people of all racial groups and socioeconomic backgrounds, some groups appear to have a higher prevalence of the condition. The likelihood of a child being diagnosed with FASD increases with a mother who is unemployed, non-Hispanic, possesses no high school degree, receives Medicaid, and has a history of mental illness and/ or substance use disorders (Wilkoit et al., 2017). The health behavior of the mother and the fetus’s ability to metabolize alcohol both play a role in the development of FASD.
Education
Primary prevention through early interventions is vital to lowering the incidence of children born with FASD. Increasing birth control and reducing alcohol consumption decreases the risk of a child born with FASD. However, the key to prevention is through education. Studies found that motivational interviewing exhibited the most positive behavioral changes to at-risk mothers (Jacobsen et al., 2022). Programs such as CHOICES use motivational interviewing to target women who are not pregnant but consume high levels of alcohol to consume less alcohol and use contraceptives (CDC, 2022). Other education methods regarding FASD include educational posters in public places, educational workshops, and warning signs on alcohol bottles (Jacobsen et al., 2022). Education is important to the prevention of FASD. However, in the occurrence of an FASD diagnosis, methods of intervention may be required.
Intervention
The effects of alcohol on a fetus are irreversible, and currently, no treatment exists. However, measures to reduce the effects of alcohol exposure during pregnancy exist and vary between individuals. Methods to assist a child with FASD include a stable home environment, positive connections to social services, reduced exposure to violence, and a diagnosis before age six (CDC, 2022). Children with FASD should be referred to child psychologists, pediatricians, and/or doctors specializing in genetics. The combination of medical intervention and a caring support system can help reduce the FASD effects on child development.
Conclusion
Throughout American history, alcohol has been one of the most popular and consumed drugs. However, it was not until the 1970s that scientists discovered the harmful effects of alcohol on the developing fetus. The newfound studies on the impacts of fetal alcohol exposure on behavior, cognition, and emotional regulation in childhood became a public health concern. Today, the CDC states there is no safe time to consume alcohol during pregnancy (CDC, 2023). Therefore, alcoholic beverages should be completely avoided if a woman is pregnant or trying to become pregnant in order to reduce the incidence of FASD. Education and an increase in public awareness are essential to preventing children born with FASD.
Review Questions
1. True or false: alcohol is considered a teratogen.
a. True
b. False
2. Alcohol exposure during pregnancy can lead to:
a. Cognitive delays
b. Physical abnormalities
c. Behavioral delays
d. All of the above
3. Which of the following refers specifically to the mental health effects of prenatal alcohol exposure?
a. Fetal Alcohol Syndrome
b. Alcohol-Related Neurodevelopmental Disorder
c. Alcohol-Related Birth Defects
d. Neurobehavioral Disorder Associated with prenatal alcohol exposure
References
Armstrong E. M. (1998). Diagnosing moral disorder: the discovery and evolution of fetal alcohol syndrome. Social science & medicine (1982), 47(12), 2025–2042. https://doi.org/10.1016/s0277-9536(98)00308-6
Armstrong, E. M., & Abel, E. L. (2000). Fetal alcohol syndrome: the origins of a moral panic. Alcohol and alcoholism (Oxford, Oxfordshire), 35(3), 276–282. https://doi.org/10.1093/alcalc/35.3.276
Brown, J. M., Bland, R., Jonsson, E., & Greenshaw, A. J. (2019). A brief history of awareness of the link between alcohol and fetal alcohol spectrum disorder. Canadian Journal of Psychiatry, 64(3), 164–168. https://doi.org/10.1177/0706743718777403
Centers for Disease Control and Prevention. (2022). Fetal alcohol spectrum disorder (FASDs). https://www.cdc.gov/ncbddd/fasd/facts.html
Hagan, J. F., Jr, Balachova, T., Bertrand, J., Chasnoff, I., Dang, E., Fernandez-Baca, D., Kable, J., Kosofsky, B., Senturias, Y. N., Singh, N., Sloane, M., Weitzman, C., Zubler, J. (2016). Neurobehavioral disorder associated with prenatal alcohol exposure. Pediatrics, 138(4), e20151553. https://doi.org/10.1542/peds.2015-1553
Jacobsen, B., Lindemann, C., Petzina, R., & Verthein, U. (2022). The universal and primary prevention of foetal alcohol spectrum disorders (FASD): a systematic review. Journal of Prevention, 43(3), 297–316. https://link.springer.com/article/10.1007/s10935-021-00658-9
Sambo, D., & Goldman, D. (2023). Genetic influences on fetal alcohol spectrum disorder. Genes, 14(1). https://doi.org/10.3390/genes14010195
Stanford Health Children’s Medicine. (2022). Alcohol and pregnancy. https://www.stanfordchildrens.org/en/topic/default?id=alcohol-and-pregnancy-85-P01188
Wilhoit, L.F., Scott, D.A. & Simecka, B.A. Fetal alcohol spectrum disorders: characteristics, complications, and treatment. Community Mental Health J 53, 711–718 (2017). https://doi.org/10.1007/s10597-017-0104-0
a group of conditions that can occur in a person who was exposed to alcohol before birth
a drug initially used to treat a range of conditions (morning sickness, flu, etc.) in the 1960s until it was found to cause severe physical deformities in babies during pregnancy
physicians who are concerned with abnormal fetal development
a condition in a child that results from alcohol exposure before birth and is characterized by limited mental development and physical growth
the collection of injuries sustained by a child as a result of repeated mistreatment or abuse
a medical condition characterized by having intellectual disabilities and problems with behavior and learning as a result of alcohol exposure before birth
medical conditions linked to alcohol exposure before birth; consist of heart and bone malformations, difficulty seeing and hearing, and a reduced immune function
a group of conditions related to behavioral challenges associated with brain impairments, injuries, or diseases
an agent or factor that causes developmental malformations during pregnancy
the organ that unites the fetus to the maternal uterus and allows for exchange of nutrients
the fluid that surrounds and protects the fetus during pregnancy
area of the brain responsible for memory
area of the brain responsible for emotions
of, relating to, or involving a combination of social and economic factors
proportion of a population with a disease or condition
the breakdown of chemical substances; the sum of processes that provide the body with energy
the occurrence of new cases
a counseling approach designed to enhance someone's motivation to change
also called birth control, they are the methods, medicines, and devices used to prevent pregnancy

