4 From Roots to Reach: Social Factors in Childhood Obesity
Sabrina Hayslett
This chapter is based on the Social Ecological Model.
Childhood obesity is a long-term (chronic) condition that occurs when a child is above a healthy weight for their age, height, and sex assigned at birth (Cleveland Clinic, 2024). Doctors classify children aged two and older as obese when their body mass index (BMI) reaches or exceeds the 95th percentile for their age and sex (Cleveland Clinic, 2024). BMI measures for obesity and potential health risks (World Health Organization [WHO], 2024). A high BMI can harm health and is associated with long-term health issues like heart disease, type 2 diabetes, and high blood pressure, which can affect bone health, reproduction, and overall quality of life (WHO, 2024). According to the CDC, 19.7% of children and adolescents in the United States are overweight or obese (Cleveland Clinic, 2024). A BMI of over 25 characterizes overweight as a condition of excessive fat deposits (WHO, 2024). A BMI over 30 and excessive fat deposits that harm health define obesity as a chronic disease (WHO, 2024).
A child has a higher obesity risk due to:
- Mother’s Health During Pregnancy: Pregnant women with insulin resistance or gestational diabetes are more likely to have children at risk for obesity (Obesity Medicine Association [OMA], 2021). High blood sugar during pregnancy can increase the baby’s insulin levels, leading to greater birth weight (OMA, 2021).
- Genetic Factors: Obesity can run in families due to genetics, and hormonal disorders can also lead to weight gain (OMA, 2021).
- Diet: Eating too often, consuming large portions, and choosing highly processed foods can lead to excessive calorie intake and weight gain (Mayo Clinic, 2025).
- Lack of Movement: Children living sedentary lifestyles, with insufficient daily physical activity, are at higher risk of obesity (Mayo Clinic, 2025). Excess screen time replaces active play and contributes to weight gain (UCSF, n.d.). Sitting for extended periods is linked to metabolic syndrome and other chronic diseases (Barnett et al., 2018). Children and teens should aim for 9,000 to 12,000 steps daily to support healthy physical activity levels (Tresca, 2024).
- Environmental Factors: A child’s diet depends on what their parents provide. Limited access to nutritious meals and reliance on high-calorie, low-nutrient foods increase obesity risk (Cleveland Clinic, 2024). Social determinants of health, such as safe places for physical activity, also play a role (Cleveland Clinic, 2024). Parks and playgrounds are critical for promoting active lifestyles (Cleveland Clinic, 2024).
Addressing childhood obesity prevents long-term health complications, reduces healthcare costs, and improves quality of life, both physically and emotionally. Early interventions that promote healthy eating and physical activity establish lifelong habits for children and reduce obesity risks for future generations.
Individual
Children facing obesity not only struggle with maintaining physical health but also face emotional and social challenges, including low self-esteem, bullying, and difficulty forming friendships, all of which can contribute to unhealthy coping mechanisms like emotional eating and reduced physical activity (AAP, 2021).
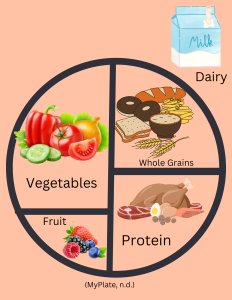
Children learning about balance and moderation can decrease weight challenges. MyPlate illustrates the balance of fruits, grains, dairy, protein, and vegetables that can be visualized on a plate (Kidsville Pediatrics, 2024). MyPlate also offers apps and games, like the Dining Decisions Mobile App, to teach kids about wise food choices engagingly (MyPlate, n.d.). When children learn to read and understand food labels, they can practice making informed food choices about nutrients and serving sizes, which will also help them as adults (Kidsville Pediatrics, 2024).
Beyond physical health, obesity affects mental well-being. Overweight children are more likely to face bullying, struggle academically, and develop low self-esteem (AAP, 2021). Stressors such as divorce, loss, or school struggles can trigger emotional eating, reinforcing unhealthy habits (Förster et al., 2023). Caregivers can help by teaching coping strategies like deep breathing, journaling, or talking to a trusted person (Affinity Health, 2023). Programs like Mindful Kids teach children mindfulness-based behavioral skills to manage emotions, build self-awareness, and develop empathy (Mindful Kids, n.d.).
Obesity can also limit participation in sports and social activities, increasing isolation and worsening self-esteem (Affinity Health, 2023). Instead of focusing on weight loss, caregivers and educators can promote healthy habits like eating, staying active, reducing screen time, and getting enough sleep (Affinity Health, 2023).
Relationship
Children who lack healthy food or have regular medical care face increased health risks. Consuming too many processed foods and sugary drinks can lead to diabetes and heart disease. At the same time, missing doctor visits makes it harder to catch early signs of obesity-related issues (CDC, n.d.a). When kids lack support, proper nutrition, and healthcare, staying healthy and managing their weight becomes even more difficult.
Parents shape their children’s habits and can help reduce obesity risk through:
- Family movement: Modeling active behavior with activities like going to the park or dancing (CDC, n.d.a).
- Sleep routines: Good sleep prevents obesity, diabetes, and behavioral issues. Limiting screens before bed improves sleep quality (CDC, n.d.a). Lack of sleep can lead to unhealthy weight gain.
- Healthy eating habits: Families can practice balanced nutrition and avoid using food as a reward (Kidsville Pediatrics, 2024). MEND (Mind, Exercise, Nutrition…Do It!) helps families of children aged 2 to 13 incorporate healthy eating, physical activity, and behavior change strategies into their lives (Healthy Weight Partnership, n.d.). Smart Moves is a similar program for families with children aged 7 to 18, but it also focuses on coping strategies, portion control, and meal preparation. (Smart Moves for Kids, n.d.). Participants in Smart Moves experienced decreased insulin resistance, decreased cholesterol, and a lower body fat percentage (National Cancer Institute, 2024).
- The role of pediatricians: Pediatricians can conduct routine BMI screenings during annual check-ups to identify children at risk for obesity early (CDC, n.d.b). They can involve parents in discussions about their child’s health and guide the family toward healthier habits (Muth et al., 2024). Pediatricians also collaborate with local organizations like the YMCA to connect families with resources for nutrition or exercise classes (Attaway, 2025).
Community
With 95% of children aged 5-17 attending schools, schools play a key role in influencing childhood nutrition (United Nations Children’s Fund, 2021). They can limit junk food, work with dietitians on healthy menus, and ensure nutrition and physical education are part of the curriculum (United Nations Children’s Fund, 2021). Programs like the Comprehensive School Physical Activity Program (CSPAP) promote physical education to address childhood obesity by building physical fitness, motor skills, and lifelong healthy habits.
Communities play a key role in reversing the childhood obesity epidemic by promoting healthy eating and creating safe spaces for physical activity. Community gardens are effective interventions, increasing access to fresh fruits and vegetables and encouraging physical activity (Stluka et al., 2019). Participation in these gardens has reduced food insecurity while offering social and emotional benefits (Stluka et al., 2019).

A child’s built environment significantly impacts their physical activity and healthy food access. Communities can enhance sidewalks, parks, bike trails, and green spaces, all of which help protect children from obesity (Sridhar & Gumpeny, 2024). In neighborhoods with high crime rates, outdoor activity is often limited, which increases obesity risk (Sridhar & Gumpeny, 2024). Supermarkets with healthy food options, walkability, and social cohesion are protective factors against weight gain (Daniels et al., 2021).
Communities with socioeconomic challenges tend to have higher childhood obesity rates (Daniels et al., 2021). Creating supportive and safe neighborhood environments is essential to encourage healthier lifestyles and reduce obesity rates (Daniels et al., 2021). The CEE Greenville Boxing Club, located in Greenville, SC, is a nonprofit organization that combines boxing training with academic enrichment to support local youth (Clayton, 2024). This program helps children build confidence, develop a positive mindset, and improve physical and emotional well-being (Clayton, 2024).
Societal
While many families in the U.S. struggle to afford nutritious foods, fast food and processed snacks are widely accessible and advertised to children. Schools and government programs work to provide healthier meals, but disparities in food security and nutritional education remain. For more information on food insecurity, refer to this chapter.
The U.S. Department of Agriculture (USDA) oversees federally assisted meal programs that promote healthy eating in schools. The School Breakfast Program (SBP) funds low-cost or free breakfasts for 14.6 million children annually. In comparison, the National School Lunch Program (NSLP) provides lunches and snacks to over 30 million children in public and private nonprofit schools (HSPH, n.d.).
The Fresh Fruit and Vegetable Program (FFVP) introduces elementary school children to fresh produce, encouraging healthy food choices (HSPH, n.d.). The Healthy, Hunger-Free Kids Act (HHFKA) of 2010 improved the nutritional quality of meals served in the NSLP and SBP by implementing age-specific serving sizes, increasing whole grains, requiring low-fat or fat-free milk, expanding fruit and vegetable offerings, and limiting starchy vegetables (HSPH, n.d.). Since its implementation, HHFKA has helped reduce childhood obesity rates, especially among children in poverty.
The NSLP and SBP actively prevent obesity through:
- Portion control: Ensuring proper serving sizes for balanced nutrition (Food and Nutrition Service, 2024).
- Age-specific calorie limits: Help meals provide appropriate portions and prevent excessive intake that leads to obesity (CSDE, 2024).
- Balanced eating: Schools work with dietitians to create menus that follow federal guidelines and support healthy habits (Career Navigator, 2024).
Key Takeaways
- Child obesity, affecting 1 in 5 kids in the United States, is caused by factors like genetics, diet, lack of exercise, and environment, and early actions promoting healthy habits can prevent long-term health problems.
- Teaching kids about portion sizes, reading food labels, and ways to handle stress – like journaling or mindfulness – can help them make healthier choices and deal with the physical and emotional challenges of obesity.
- Caregivers play a big role in shaping children’s behaviors by modeling healthy eating, participating in physical activities as a family, establishing sleep routines, and using programs like MEND or Smart Moves to support lifestyle changes.
- Communities can fight childhood obesity by creating safe spaces for physical activity, like parks and playgrounds, starting community gardens, and making healthy food options easier to get.
- Government programs like the National School Lunch Program (NSLP), Fresh Fruit and Vegetable Program (FFVP), and policies like the Healthy, Hunger-Free Kids Act help schools serve healthier meals and lower obesity rates, especially for kids in low-income families.
- Stopping the childhood obesity epidemic needs a big effort from all levels – teaching kids, involving families, supporting communities, and creating policies – to make lasting changes and healthier lives for children.
References
Affinity Health. (2023, March 2). What impact does obesity have on a child’s psychological wellbeing? https://www.affinityhealth.co.za/what-impact-does-obesity-have-on-a-childs-psychological-wellbeing/
American Academy of Pediatrics. (2021, March 9). The emotional toll of obesity. Healthy Children. https://www.healthychildren.org/English/health-issues/conditions/obesity/Pages/The-Emotional-Toll-of-Obesity.aspx
Attaway, D. (2025, January 7). Healthy weight for youth is a family affair. Clemson News. https://news.clemson.edu/healthy-weight-for-youth-is-a-family-affair/
Barnett, T.A., Kelly, A.S., Young, D.R., Perry, C.K., Pratt, C.A., Edwards, N.M., Rao, G., & Vos, M.B. (2018). Sedentary behaviors in today’s youth: Approaches to the prevention and management of childhood obesity: A scientific statement from the American Heart Association. Circulation, 138(11). https://doi.org/10.1161/CIR.0000000000000591
Career Navigator. (2024, November 22). Registered dietitian in schools: Importance and impact. American Profession Guide. https://americanprofessionguide.com/registered-dietitians-in-schools/
Centers for Disease Control and Prevention [CDC]. (n.d.a). Preventing childhood obesity: 6 things families can do. https://www.cdc.gov/obesity/family-action/index.html
Centers for Disease Control and Prevention [CDC]. (n.d.b). Screening for childhood obesity. https://www.cdc.gov/obesity/child-obesity-screening/index.html
Clayton, J. (2024, April 1). Greenville boxing club prepares youth, inside the ring and out. South Carolina Public Radio. https://www.southcarolinapublicradio.org/sc-news/2024-04-01/greenville-boxing-club-prepares-youth-inside-the-ring-and-out
Cleveland Clinic. (2024, February 21). Childhood obesity: Causes & problems. https://my.clevelandclinic.org/health/diseases/9467-obesity-in-children
Connecticut State Department of Education [CSDE]. (2024, June). Calorie ranges for the NSLP and SBP. https://portal.ct.gov/-/media/sde/nutrition/nslp/mealpattern/calorie_ranges_nslp_sbp.pdf
Daniels, K.M., Schinasi, L.H., Auchincloss, A.H., Forrest, C.B., & Roux, A.V.D. (2021). The built and social neighborhood environment and child obesity: A systematic review of longitudinal studies. Elsevier, 153, 106790. https://doi.org/10.1016/j.ypmed.2021.106790
Food and Nutrition Service. (2024, December 4). National School Lunch Program meal pattern. USDA. https://www.fns.usda.gov/school-meals/nutrition-standards/nslp-meal-pattern
Förster, L.J., Vogel, M., Stein, R., Hilbert, A., Breinker, J.L., Böttcher, M., Kiess, W., & Poulain, T. (2023). Mental health in children and adolescents with overweight or obesity. BMC Public Health, 23(135). https://doi.org/10.1186/s12889-023-15032-z
Harvard T. H. Chan School of Public Health [HSPH]. (n.d.). Healthy schools. The Nutrition Source. https://nutritionsource.hsph.harvard.edu/healthy-schools/
Healthy Weight Partnership. (n.d.). Healthy lifestyle and weight management programs for children and families. https://healthyweightpartnership.org/
Kidsville Pediatrics. (2024, July 16). 10 smart strategies to combat childhood obesity. Children’s Health. https://www.kidsvillepeds.com/blog/1186611-10-smart-strategies-to-combat-childhood-obesity/
Mayo Clinic. (2025, January 8). Childhood obesity: Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/childhood-obesity/symptoms-causes/syc-20354827
Mindful Kids. (n.d.). Home. https://mindfulkids.me/
Muth, N.D., Bolling, C., Hannon, T., & Sharifi, M. (2024). The role of the pediatrician in the promotion of healthy, active living. Pediatrics, 153(3), e2023065480. https://doi.org/10.1542/peds.2023-065480
MyPlate. (n.d.). Nutrition information for kids. USDA. https://www.myplate.gov/life-stages/kids
National Cancer Institute. (2024, September 9). Smart Moves / Bright Bodies: Evidence-Based Cancer Control Programs (EBCCP). https://ebccp.cancercontrol.cancer.gov/programDetails.do?programId=1896571
Obesity Medicine Association. (2021, July 12). Risk factors for childhood obesity. https://obesitymedicine.org/blog/risk-factors-for-childhood-obesity-obesity-medicine-association/
Smart Moves for Kids. (n.d.). Bright Bodies at Yale. https://www.smartmovesforkids.com/bright-bodies-program-overview
Sridhar, G. R. & Gumpeny, L. (2024). Built environment and childhood obesity. World Journal of Clinical Pediatrics, 13(3), 93729. https://dx.doi.org/10.5409/wjcp.v13.i3.93729
Stluka, S., McCormack, L. A., Burdette, L., Dvorak, S., Knight, N., Lindvall, R., Pierce, L., Schoch, J., & Walkling, P. (2019). Gardening for health: Using garden coordinators and volunteers to implement rural school and community gardens. Centers for Disease Control and Prevention, 16, e190117. http://dx.doi.org/10.5888/pcd16.190117
Tresca, A.J. (2024, July 11). Targeting the average number of steps per day for your age and sex. Verywell Health. https://www.verywellhealth.com/average-steps-per-day-8671820
UCSF Benioff Children’s Hospital. (n.d.). Childhood obesity and screen time: Patient education A-Z. https://www.ucsfbenioffchildrens.org/education/childhood-obesity-and-screen-time
United Nations Children’s Fund. (2021, July). The role of schools in preventing overweight and obesity among students in Latin America and the Caribbean. UNICEF. https://www.unicef.org/lac/media/30436/file/The-role-of-schools-in-preventing-overweight.pdf
World Health Organization [WHO]. (2024, March 1). Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
A simple way to measure whether someone’s weight is healthy for their height. It’s calculated by dividing a person’s weight by their height.
Conditions that affect the heart and blood vessels, such as heart attacks, high blood pressure, and blocked arteries
Condition where the body can't use insulin properly, leading to high blood sugar levels
High blood pressure (hypertension) happens when the force of blood against the walls of the arteries is too strong.
Having more body fat than is healthy occurs when the body stores extra energy (calories) that it doesn't use, leading to a buildup of fat. Too much fat can cause health problems over time.
Reduced sensitivity to insulin by the body's insulin-dependent processes (such as glucose uptake and lipolysis) that is typical of type 2 diabetes but often occurs in the absence of diabetes
A condition characterized by an elevated blood sugar during pregnancy, typically resolving after birth
A protein pancreatic hormone secreted by the islets of Langerhans in the pancreas that is essential for the metabolism of carbohydrates and the regulation of glucose (sugar) levels in the blood and that when insufficiently produced results in diabetes mellitus
Products that go through multiple industrial processes and contain artificial ingredients like preservatives, sweeteners, and flavor enhancers. These foods are often high in sugar, unhealthy fats, and salt, and low in nutrients. Examples include soda, chips, fast food, instant noodles, and packaged desserts. Regularly eating ultra-processed foods can increase the risk of obesity, heart disease, and diabetes (World Health Organization, 2024)
Not moving enough and spending too much time sitting
A group of health problems that happen together. It includes high blood pressure, high blood sugar, extra fat around the belly, and unhealthy cholesterol levels. Having metabolic syndrome increases the risk of getting diseases like diabetes, heart disease, and stroke.
Nonmedical factors that influence health outcomes; the conditions in which people are born, grow, work, live, worship, and age
A person’s sense of their own value or worth.
Ways people deal with stress, emotions, or difficult situations. They help manage feelings like anxiety, sadness, or frustration in a healthy way. Some good coping strategies include deep breathing, talking to a friend, exercising, or writing in a journal.
A fat-like substance found in the blood that helps the body build cells, hormones, and vitamins. Too much cholesterol can clog arteries.
The amount of fat in your body compared to everything else, like muscles, bones, and water.
Of, relating to, or involving a combination of social and economic factors
A trained expert in nutrition and healthy eating. They help people choose the right foods to manage their health, prevent diseases, and reach personal wellness goals. Dietitians work in hospitals, schools, and clinics to guide individuals on balanced diets for different needs.

