8 More Than a Birthweight: Reducing Fetal Macrosomia
Sophia Miller
This chapter is based on the Social Ecological Model.
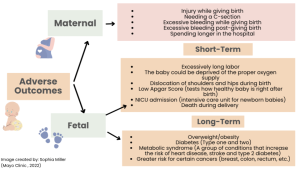
Fetal macrosomia can lead to serious health problems for both mother and baby (Means & Means, 2024). These overweight babies may experience low blood sugar, breathing difficulties, and long-term health issues (Mayo Clinic, 2022). Mothers may go through difficult labor, require a cesarean (C) section, or experience heavy bleeding after delivery (Mayo Clinic, 2022).

Although predicting fetal macrosomia can be challenging, doctors identify several common causes. These include gaining too much weight during pregnancy, having diabetes or gestational diabetes, measuring a large fundal height, carrying the pregnancy past the due date, previously giving birth to a large baby, or having been a large baby at birth yourself (Cleveland Clinic, 2022). Among these, gestational diabetes and obesity are the most frequent contributors (Cleveland Clinic, 2022). Expectant mothers should follow a healthy lifestyle by eating balanced meals and staying active (Marshall et al., 2021). To lower the risk of macrosomia, pregnant individuals should attend regular prenatal appointments, gain a healthy amount of weight during pregnancy, and manage diabetes effectively if diagnosed (Mayo Clinic, 2022). Fetal macrosomia can lead to both immediate and long-term complications for mothers and infants. See image below:
Living a healthy lifestyle during pregnancy helps reduce the risk of macrosomia and its related complications.
Individual
Pregnant individuals can lower their risk of fetal macrosomia by focusing on personal health. A healthy diet is important—eating whole grains, lean protein, fruits, and vegetables can help control blood sugar levels and prevent excessive weight gain (Chalas, 2020). Regular exercise, like walking or swimming, also lowers the risk of excessive fetal growth (Wang et al., 2019). Managing stress through relaxation techniques can also improve pregnancy health (Pan et al., 2023). Staying active, eating well, and reducing stress all help lower the chances of having a baby with macrosomia. March of Dimes recommends several practices for optimal health.
Mobile health apps teach and encourage pregnant individuals to stay healthy, helping reduce the risk of fetal macrosomia (Sandborg et al., 2021). One example is the HealthyMoms smartphone app, which promotes healthy weight gain, good nutrition, and regular activity during pregnancy without harming the baby (Sandborg et al., 2021). Researchers have evaluated the app’s effectiveness in several trials. While the app does not work the same for all body mass index (BMI) groups, it has successfully helped reduce excessive weight gain during pregnancy and encourages a healthy lifestyle through education (Sandborg et al., 2021). This app is widely available for download through most mobile app stores.
Maternal depression is a lesser-known cause of fetal macrosomia. “… maternal depression during early pregnancy is significantly associated with increased fetal growth, higher birth weight, and elevated risk of macrosomia and severe large for gestational age after birth.” (Wu et al., p.813). Fetal growth changes throughout pregnancy. For example, head length growth occurs after 32 weeks, whereas abdominal circumference increases before 23 weeks (Wu et al., 2024). The timing and strength of maternal depression can affect the development of these structures (Wu et al., 2024). People who are depressed tend to exercise less and eat more calorie-dense foods. Pregnant individuals should talk to their provider if they notice any signs of depression.
Relationship
Support from family, friends, and doctors can help encourage pregnant individuals to stay on track with healthy habits. Loved ones can motivate pregnant individuals to eat nutritious foods and remain physically active. A 2021 meta-analysis in the Journal of the American Medical Association (JAMA) found that lifestyle counseling and behavioral support during pregnancy lowered the risk of gestational diabetes and fetal macrosomia (Cantor et al., 2021). Doctors and nurses also monitor the baby’s growth and offer personalized advice on diet and exercise. When pregnant individuals communicate openly and regularly with their healthcare providers, it is easier to follow recommendations and avoid complications.
Telehealth services support many individuals who struggle to access care, especially quality or specialty care. A 2020 study found that for pregnant women with gestational diabetes mellitus (GDM), telemedicine worked better than regular care at lowering blood sugar levels (Xie et al., 2020). Telehealth also helps reduce the risk of complications for both mother and baby during and after pregnancy (Xie et al., 2020). Telehealth provides expecting and new mothers a practical “how-to” guide for accessing care remotely while maintaining strong connections with their healthcare providers. The guide explains what telehealth is, outlines its benefits for pregnant women, and offers instructions on how to use it, including the tools needed (Health Resources and Services Administration, 2024). Telehealth makes it easier for patients and providers to stay connected, even from far away. Studies show that stronger relationships between patients and providers lead to more prenatal visits and fewer pregnancy problems (Roberts et al., 2015).
Community
Community programs and resources support healthy habits during pregnancy. Exercise programs designed for pregnancy can help reduce the risk of excessive fetal growth (American College of Obstetricians and Gynecologists, 2020). Nutrition classes teach expectant mothers to develop healthy eating habits—a key step since many do not meet nutrition guidelines (Habbal et al., 2023).
The Motherhood Center (New York, NY-based) offers in-person and online mental health services and support groups. The program provides nutritional counseling and mental health support, which helps prevent fetal macrosomia. Wellness programs that include cognitive behavioral therapy can empower mothers to make healthier choices during pregnancy and feel emotionally supported before birth. Licensed perinatal therapists lead virtual support groups that cover topics like general pregnancy care and coping with past depression or anxiety (The Motherhood Center, 2025). Support groups and therapy play a big role in lowering the risk of pregnancy complications, including macrosomia. Each session costs about $25. Although free support groups are harder to find, helpful resources like webinars and written advice are available for those in need.
An example of a helpful community-based program is Moms2B, based in Columbus, Ohio (Gabbe et al., 2017). This program provides prenatal education, nutrition support, and group sessions, especially for women living in underprivileged urban communities (Gabbe et al., 2017; Hade et al., 2021). While fetal macrosomia rates were not directly measured, “most of the women said they learned to eat healthier, to be more physically active, and to follow their health care provider’s recommendations” (Gabbe et al., 2017, p. 1135). Moms2B may help reduce the risk of macrosomia by promoting healthy weight gain and balanced nutrition (Gabbe et al., 2017; Hade et al., 2021).
Societal
Fetal macrosomia rates are directly influenced by healthcare policies and government programs. “One reason that prenatal care is not fully accessible to poor populations is the relative lack of private obstetrical services for women relying on Medicaid” (Committee to Study the Prevention of Low Birthweight et al., 1985). Since obesity and gestational diabetes increase the risk of macrosomia, early screening programs are important because they help identify and manage these conditions more effectively (American Diabetes Association, 2020; Gabbe et al., 2017). Access can be improved by encouraging more doctors to accept Medicaid.
In her book Good Energy, Dr. Casey Means (2024) explains that at-home monitoring devices can help pregnant individuals manage blood sugar levels and reduce the risk of gestational diabetes. When used alongside telemedicine, these tools allow healthcare providers to monitor patients remotely—an advantage for high-risk pregnancies that need close care (Weigel & Frederiksen, 2020). However, these devices can be costly and are not always covered by insurance. Coverage for telemedicine services and remote monitoring devices like continuous glucose monitors (CGMs) depends on the type of insurance. Some insurance plans only approve CGM use if the patient already has diabetes, which limits access for pregnant individuals at risk of developing gestational diabetes (Weigel & Frederiksen, 2020). Without affordable options, many patients miss out on tools that can prevent fetal macrosomia and other problems. Self-advocacy is essential, and pregnant individuals should ask their providers about monitoring options and push for insurance coverage when necessary (Means & Means, 2024).
Telehealth and mobile health services make it easier for more pregnant people to get care and support during pregnancy (Hawkins, 2023; Weigel & Frederiksen, 2020). A 2023 study found that mobile health tools significantly helped prevent gestational diabetes in overweight or obese pregnant individuals (He et al., 2024). March of Dimes, a nationwide initiative, supports at-risk pregnant individuals by offering maternal health programs, especially in areas with limited care (March of Dimes, 2023). The organization reports that “more than 5.6 million women of childbearing age in the U.S. live in counties with limited or no access to maternity care. March of Dimes Mom & Baby Mobile Health Centers help address the problem by providing care to those who need it” (March of Dimes, 2023). Public health advocates should help all pregnant individuals find quality prenatal care to prevent issues like macrosomia.
Key Takeaways
- Healthy eating, regular exercise, and stress reduction techniques can significantly lower the risk of fetal macrosomia.
- Support from relationships, including family, friends, and healthcare providers, encourages positive health behaviors and effective prenatal care.
- Community resources such as nutrition classes, prenatal exercise programs, and mobile health apps offer education and support for healthy pregnancies.
- Larger efforts like early screening for gestational diabetes, expanded prenatal care, and public health campaigns help reduce fetal macrosomia rates.
- With rising obesity, it is more important than ever for pregnant people to stay healthy—giving their babies a strong start and breaking the cycle of poor health.
References
American College of Obstetricians and Gynecologists. (2020). Macrosomia. Obstetrics & Gynecology, 135(1), e18–e35. https://doi.org/10.1097/aog.0000000000003606
American Diabetes Association. (2019). 11. Microvascular complications and foot care: Standards of medical care in diabetes−2020. Diabetes Care, 43(Supplement 1), S135–S151. https://doi.org/10.2337/dc20-s011
Cantor, A. G., Jungbauer, R. M., McDonagh, M., Blazina, I., Marshall, N. E., Weeks, C., Fu, R., LeBlanc, E. S., & Chou, R. (2021). Counseling and Behavioral Interventions for Healthy Weight and Weight Gain in Pregnancy: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA, 325(20), 2094–2109. https://doi.org/10.1001/jama.2021.4230
Chalas, E. (2020). The American College of Obstetricians and Gynecologists in 2020: A Clear Vision for the Future. Obstetrics and Gynecology, 135(6), 1251–1254. https://doi.org/10.1097/AOG.0000000000003899
Cleveland Clinic. (2022, May 13). Fetal Macrosomia: What Is It, Causes & Outlook. https://my.clevelandclinic.org/health/diseases/17795-fetal-macrosomia
Committee to Study the Prevention of Low Birthweight, Division of Health Promotion and Disease Prevention, & Institute of Medicine. (1985). Ensuring access to prenatal care. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK214476/
Gabbe, P.T., Reno, R., Clutter, C. (2017) Improving maternal and infant child health outcomes with community-based pregnancy support groups: Outcomes from Moms2B Ohio. Maternal Child Health Journal 21, 1130–1138 . https://doi.org/10.1007/s10995-016-2211-x
Hade, E. M., Lynch, C. D., Benedict, J. A., Smith, R. M., Ding, D. D., Gabbe, S. G., & Gabbe, P. T. (2021). The association of Moms2B, a community-based interdisciplinary intervention program, and pregnancy and infant outcomes among women residing in neighborhoods with a high rate of infant mortality. Maternal and Child Health Journal, 26(4). https://doi.org/10.1007/s10995-020-03109-9
Hawkins, S. S. (2023). Telehealth in the prenatal and postpartum periods. Journal of Obstetric, Gynecological & Neonatal Nursing. 52(4). 264-275 https://doi.org/10.1016/j.jogn.2023.05.113
He, Y., Huang, C., He, Q., Liao, S., & Luo, B. (2024). Effects of mHealth-based lifestyle interventions on gestational diabetes mellitus in pregnant women with overweight and obesity: systematic review and meta-analysis. JMIR Mhealth and Uhealth, 12, e49373–e49373. https://doi.org/10.2196/49373
Health Resources and Services Administration. (2024). How can I use telehealth during and after pregnancy? https://telehealth.hhs.gov/patients/how-can-i-use-telehealth-during-and-after-pregnancy#what-is-telehealth-for-maternity-care
March of Dimes. (2023). March of Dimes Mom & Baby Mobile Health Centers. https://www.marchofdimes.org/our-work/mobile-health-centers
Marshall, N. E., Abrams, B., Barbour, L. A., Catalano, P., Christian, P., Friedman, J. E., Hay, W. W., Hernandez, T. L., Krebs, N. F., Oken, E., Purnell, J. Q., Roberts, J. M., Soltani, H., Wallace, J., & Thornburg, K. L. (2021). The importance of nutrition in pregnancy and lactation: Lifelong consequences. American Journal of Obstetrics and Gynecology, 226(5), 607–632. https://doi.org/10.1016/j.ajog.2021.12.035
Mayo Clinic. (2022, June 3). Fetal macrosomia. https://www.mayoclinic.org/diseases-conditions/fetal-macrosomia/symptoms-causes/syc-20372579
Means, C. & Means, C. (2024). Good energy: The surprising connection between metabolism and limitless health. Penguin Publishing Group.
Roberts, J., Sealy, D., Marshak, H. H., Manda-Taylor, L., Gleason, P., & Mataya, R. (2015). The patient-provider relationship and antenatal care uptake at two referral hospitals in Malawi: A qualitative study. Malawi Medical Journal, 27(4), 145. https://pmc.ncbi.nlm.nih.gov/articles/PMC4761706/
Sandborg, J., Henriksson, P., Larsen, E., Lindqvist, A.-K., Rutberg, S., Söderström, E., Maddison, R., & Löf, M. (2021). Participants’ engagement and satisfaction with a smartphone app intended to support healthy weight gain, diet, and physical activity during pregnancy: Qualitative study within the HealthyMoms trial. JMIR MHealth and UHealth, 9(3), e26159. https://doi.org/10.2196/26159
The Motherhood Center. (2022, November 3). Perinatal Day Program. https://themotherhoodcenter.com/day-program/
Weigel, G., & Frederiksen, B. (2020, February 26). Telemedicine and Pregnancy Care. The Henry J. Kaiser Family Foundation. https://www.kff.org/womens-health-policy/issue-brief/telemedicine-and-pregnancy-care/
Wu, J., Zhou, F., Wang, Y., Niu, Y., Zhang, C., Meng, Y., Hao, Y., Yu, W., Liu, H., Li, C., Zhang, S., Chen, S., Xia, X., Wu, Y., & Huang, H. (2024). Associations between maternal early pregnancy depression and longitudinal fetal growth. Journal of Affective Disorders, 362, 808–815. https://doi.org/10.1016/j.jad.2024.07.068.
Xie, W., Dai, P., Qin, Y., Wu, M., Yang, B., & Yu, X. (2020). Effectiveness of telemedicine for pregnant women with gestational diabetes mellitus: an updated meta-analysis of 32 randomized controlled trials with trial sequential analysis. BMC Pregnancy and Childbirth, 20(1). https://doi.org/10.1186/s12884-020-02892-1
A condition where a baby is larger than normal at birth, usually weighing over 8 pounds, 13 ounces, regardless of how long the pregnancy lasts.
A type of surgery where a baby is born through a cut made in the mother’s belly and uterus, instead of being born through the birth canal. Doctors do this when it's safer for the mother or baby.
A condition characterized by an elevated blood sugar during pregnancy, typically resolving after birth
The length of the uterus from top to bottom during pregnancy. Length should correspond with the pregnancy weeks.
Meaning "before birth." This describes the time during pregnancy when the baby is growing in the womb.
A measure of body fat that is the ratio of the weight of the body in kilograms to the square of its height in meters
Depression that happens during pregnancy or after giving birth, affecting a mother’s mood and health.
The number of weeks a mother is in her pregnancy
The time right before or after birth
Doctors that specialize in pregnancy. These services are not funded by government, but an individual business.
A medical device attached to the skin to measure the amount of blood sugar at any given time.

