17 Allergies in Children
Alicia Moylan
Introduction
Allergy rates are steadily increasing in the United States. They are one of the most common chronic diseases, affecting nearly 40% of children (Asthma and Allergy Foundation of America, 2015). The most common types of allergies are food-based, environmental (i.e., insects, pollen, pets, and mold), and drug-based (Asthma and Allergy Foundation of America, 2015). Allergies result from an immune response that identifies a particular substance, called an allergen, as harmful and causes reaction symptoms (Mayo Clinic, 2020). Caring for a child with allergies requires understanding each type of allergy, risk factors for developing allergies, types of reactions, and available treatments.
Risk Factors and Prevention
Allergies develop from both individual exposures and genetics. Parents can reduce the risk of their child developing allergies by taking certain preventative measures prenatally and in early childhood. Metzler et al. (2019) designed a study comparing the effects of prenatal antibiotic exposure and antibiotic exposure during the first year of life on the development of allergies. They also assessed exposure to pets, smoking, and length of time breastfeeding. Prenatal and first-year-of-life antibiotic exposure was significantly correlated with developing atopic dermatitis within six years and developing a food allergy between ages 3 and 5. There was also an increased risk of seasonal and food allergen sensitivity in children exposed to antibiotics before birth (Metzler et al., 2019). Pregnant women should be aware of their antibiotic use and attempt to reduce their infant’s exposure to infections requiring antibiotics.
A mother’s diet transfers to the baby through breast milk (Venter et al., 2020). Exposure to certain foods influences the baby’s immune system and allergy development. Current guidelines tell moms not to avoid foods unless she is allergic. However, consuming fish that are rich in omega-3 fatty acids are protective against allergies (Venter et al., 2020). Similarly, foods high in vitamins A and D, nuts, dairy, and probiotic foods were all found to reduce allergic rhinitis in the baby (Venter et al., 2020). Prenatal intake of various minerals can reduce the risk of child eczema (Venter et al., 2020).
Where a child lives and their family’s income level can increase the risk of allergy formation. Allergic diseases and asthma prevalence are higher in Western, industrialized countries (Uphoff et al., 2015). In a global studies review, 66% reported that higher socioeconomic status (SES) was associated with higher prevalence rates of allergies, particularly allergic rhinitis and skin reactions. When area-level SES was reported, lower SES was linked to greater hospital admissions for anaphylactic shock (Uphoff et al., 2015).
Food Allergies
Ninety percent of food allergies are caused by milk, eggs, wheat, soy, tree nuts, peanuts, fish, and shellfish. The top three allergies in children are milk, eggs, and peanuts (Johns Hopkins Medicine, 2022). There is no medication to prevent a food allergy, so treatment involves avoiding exposure, monitoring nutritional status, and carrying an emergency kit usually containing epinephrine. With direction from the doctor, caregivers may gradually introduce foods to the child to see if they have outgrown an allergy 3 to 6 months after diagnosis (Johns Hopkins Medicine, 2022).
While homemade meals are under direct control, there are guidelines for dining out to limit allergen exposure:

Environmental & Drug Allergies
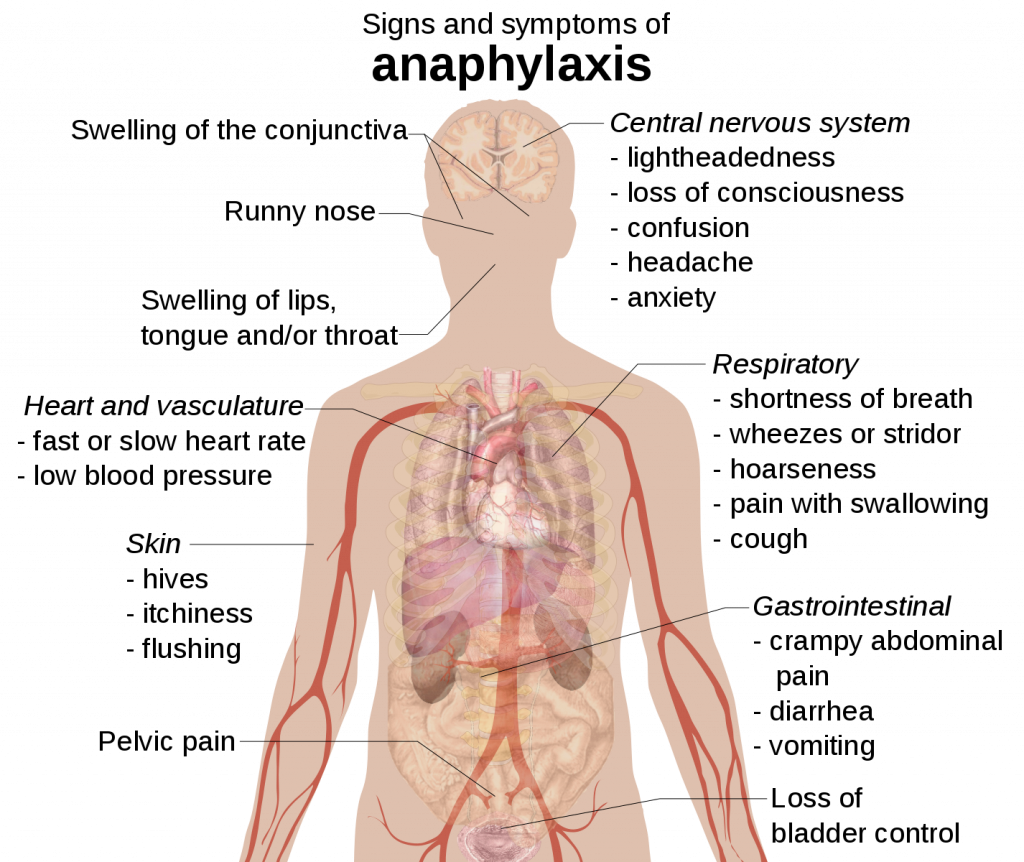
Environmental allergens include grasses, trees, pollen, insects, dust, mold, and pet hair. Managing environmental allergies mainly involves avoidance, as insect stings often cause anaphylactic shock. Environmental allergies commonly cause an itchy or runny nose, congestion, and itchy or watery eyes and occur seasonally (American College of Allergy, Asthma & Immunology, n.d.). Drug allergies are severe, affecting up to 20% of hospitalized patients (Asthma and Allergy Foundation of America, 2021). Caregivers must notify their child’s doctor of any drug allergies before any new medications are administered or prescribed. They should also be aware of the types of reactions that may occur so that they can intervene properly.
Allergy Testing
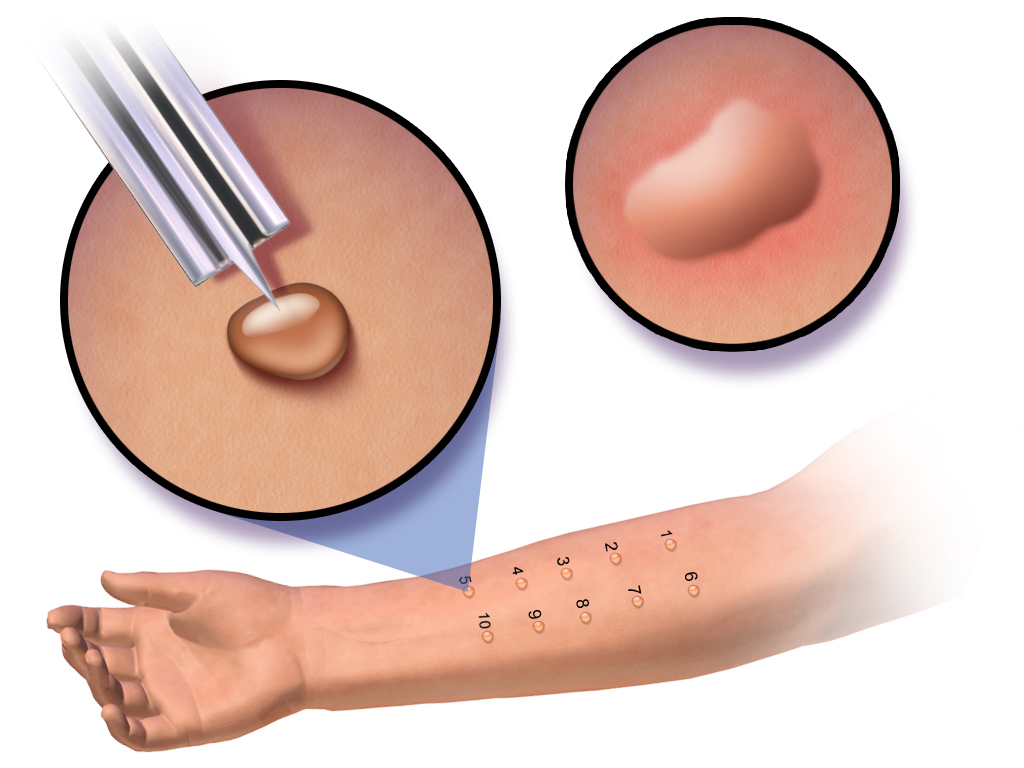
If a parent suspects the child has an allergy, there are several non-invasive tests that the child’s doctor can perform to determine the specific allergen. One of the most common testing methods is a skin test. During a skin test, small amounts of liquid containing different allergens are applied to the surface of the child’s skin with a slight scratch. A positive allergic reaction causes a small, itchy bump to appear at the application site (Cincinnati Children’s Hospital Medical Center, 2021). These results will appear within 15-20 minutes, the doctor will measure the reaction area, and itching will subside in the next half hour.
A blood test measures the child’s type and level of antibodies (Cincinnati Children’s Hospital Medical Center, 2021). Typically, a high number of specific antibodies in the blood indicates an allergy to that substance. The third most common form of testing is a graded food challenge test. Children eat a small portion of the suspected allergen and are observed for signs of a reaction (Cincinnati Children’s Hospital Medical Center, 2021). They are given gradually larger portions of that food and monitored until they eat a whole serving or the doctors intervene. Drug allergies are tested by skin tests or oral graded methods like the food challenge. Testing for drug allergies needs to occur under close observation in a doctor’s office (Cincinnati Children’s Hospital Medical Center, 2021).
Treatment
The best way to prevent allergy symptoms is to avoid the allergens as much as possible. Caregivers should remove trigger foods and household irritants. To manage symptoms caused by allergies, one can use over-the-counter (OTC) antihistamines, nose sprays, and steroid creams depending on the reaction. To determine the appropriate remedy, read more here.
Epinephrine comes in a pre-measured, injectable form as an EpiPen to use in the case of severe anaphylaxis. In an emergency, call 911 and issue epinephrine immediately. Immunotherapy is also a long-term treatment option. It is available in the form of shots and sublingual medication. Immunotherapy provides gradually larger doses of the allergen to improve tolerance of the substance and reduce symptoms and reactivity. Shots are effective for environmental allergens but not for food and drug allergies (Asthma and Allergy Foundation of America, 2018).
Resources
Management of childhood allergies and asthma involves awareness of potential exposures and a plan for relieving symptoms and preventing severe reactions. Parents, caregivers, and teachers can be proactive by teaching children about avoiding their allergen and how to get help when they have a reaction. Children’s reactions will differ in type and severity, so they may turn to friends or other supervising adults for help when they have been exposed.
- Asthma and Allergy Foundation of America
- The Asthma and Allergy Foundation of America has listed important steps to take when preparing to send a child with allergies or asthma to school. It includes forms to submit to the school and instructions on creating an action plan.
- Anaphylaxis Campaign
- The Anaphylaxis Campaign was created to support those with severe allergies, providing educational materials and community opportunities. This link advises caregivers on how to help the child understand their food allergy, refuse trigger foods, and address bullying.
- Reducing Allergens in the Home
- The Children’s Hospital of Philadelphia lists ways to limit exposure to common environmental allergens in the home such as dust mites, pollen, and mold.
- DIY Allergy Relief Kit
- List of supplies and OTC medications that should be included in an allergy kit as well as some natural remedies
Key Takeaways
- Allergies affect a large number of children and can be triggered by foods, environmental substances, and/or drugs that cause an immune response.
- Expecting mothers can reduce the risk of their child developing allergies by limiting their use of antibiotics and consuming foods with protective factors like vitamins, minerals, omega-3 fatty acids, and probiotics.
- Caregivers can learn to recognize the signs and symptoms of allergic reactions so they can intervene and consider proper allergy testing.
- The main ways to manage a child’s allergy symptoms are to avoid exposure to the allergen and to have over-the-counter medications and epinephrine available in case of a reaction.
References
AAFA Community Services. (2021, July 2). Summer to-dos before you send your child with asthma or allergies to school. https://community.aafa.org/blog/summer-to-dos-before-you-send-your-child-with-asthma-or-allergies-school?_gl=1*1u544d9*_ga*NDMzNDc3MTMxLjE2NTA4MzA2MzI.*_ga_8P8PELBV30*MTY1MDgzMDYzMS4xLjEuMTY1MDgzMDc4NC4w
American College of Allergy, Asthma & Immunology. (n.d.). Children: A child who sneezes or coughs a lot, who frequently develops a rash or hives, or who gets a stomachache, cramps or nausea after eating certain foods may have allergies. https://acaai.org/allergies/allergies-101/who-gets-allergies/children/
Anaphylaxis Campaign. (n.d.) Letting go: Teaching an allergic child responsibility. https://www.anaphylaxis.org.uk/2016/11/25/letting-go-teaching-allergic-child-responsibility/
Asthma and Allergy Foundation of America. (2015, September). Allergy overview. https://www.aafa.org/allergies.aspx#:~:text=An%20allergy%20occurs%20when%20the,These%20antibodies%20respond%20to%20allergens
Asthma and Allergy Foundation of America. (2018). Allergy treatment. https://www.aafa.org/allergy-treatments/
Asthma and Allergy Foundation of America. (2021, April). Allergy facts and figures. https://www.aafa.org/allergy-facts/
Children’s Hospital of Philadelphia. (2009, February). Controlling your home environment to prevent asthma flares. https://www.chop.edu/health-resources/controlling-your-home-environment-prevent-asthma-flares
Cincinnati Children’s Hospital Medical Center. (2021). Allergy diagnostic procedures and treatment. https://www.cincinnatichildrens.org/health/a/allergy
Johns Hopkins Medicine. (2022). Food allergies in children. https://www.hopkinsmedicine.org/health/conditions-and-diseases/food-allergies-in-children
Mayo Clinic Staff. (2020, August 4). Allergies. Mayo Foundation for Medical Education and Research. https://www.mayoclinic.org/diseases-conditions/allergies/symptoms-causes/syc-20351497
Metzler, S., Frei, R., Schmaußer, H. E., von Mutius, E., Pekkanen, J., Karvonen, A. M., Kirjavainen, P. V., Dalphin, J., Divaret, C. A., Riedler, J., Lauener, R., Roduit, C., Hyvärinen, A., Sami, R., Roponen, M., Chauveau, A., Dalphin, M., Kaulek, V., Ege, M., & Genuneit, J. (2019). Association between antibiotic treatment during pregnancy and infancy and the development of allergic diseases. Pediatric Allergy & Immunology, 30(4), 423–433. https://doi-org.libproxy.clemson.edu/10.1111/pai.13039
Piekarski, B. (2021, May 26). DIY allergy relief kit. U.S. Home Filter. https://ushomefilter.com/diy-allergy-relief-kit/
Uphoff, E., Cabieses, B., Pinart, M., Valdés, M., Antó, J. M., & Wright, J. (2015). A systematic review of socioeconomic position in relation to asthma and allergic diseases. The European Respiratory Journal, 46(2), 364-374. https://doi.org/10.1183/09031936.00114514
Venter, C., Agostoni, C., Arshad, S. H., Ben, A. M., Du Toit, G., Fleischer, D. M., Greenhawt, M., Glueck, D. H., Groetch, M., Lunjani, N., Maslin, K., Maiorella, A., Meyer, R., Antonella, M., Netting, M. J., Ibeabughichi Nwaru, B., Palmer, D. J., Palumbo, M. P., Roberts, G., & Roduit, C. (2020). Dietary factors during pregnancy and atopic outcomes in childhood: A systematic review from the European Academy of Allergy and Clinical Immunology. Pediatric Allergy & Immunology, 31(8), 889–912. https://doi-org.libproxy.clemson.edu/10.1111/pai.13303
a common chronic condition that leads to redness and irritation of the skin, and mostly occurs when individuals experience an allergic reaction
polyunsaturated fatty acids that reduce the risk of inflammatory and autoimmune diseases, like atopic dermatitis and asthma, and promote many health benefits including reduced cholesterol
a condition characterized by head congestion, sneezing, tearing, and swelling of the nasal mucous membranes, caused by an allergic reaction
an inflammatory condition of the skin attended with itching and the excretion of serous matter, which is a water-like fluid
of, relating to, or involving a combination of social and economic factors
a severe and sometimes fatal allergic reaction to a foreign substance, especially a protein, as serum or bee venom, to which an individual has become sensitized, often involving rapid swelling, acute respiratory distress, and collapse of circulation
a hormone that narrows the blood vessels, increases blood pressure, stimulates the heart muscles, and relaxes the bronchi during an asthma attack
a protein created by the body's immune system to respond to antigens, or harmful substances within the body
any of certain compounds or medicines that neutralize or inhibit the effect of histamine in the body, used chiefly in the treatment of allergic disorders and colds
the brand name of a medical injecting device that delivers a dose of epinephrine, used to treat severe allergic reactions, including anaphylaxis

