18 Asthma Management in Children
Imani Hunt
Introduction
Pediatric asthma is a chronic lung disease that causes inflammation of the lungs and difficulty breathing in children (MedlinePlus, 2021). There are five existing types of asthma: extrinsic, intrinsic, nocturnal, cough-variant, and occupational. Pediatric asthma is the most common chronic lung disease that impacts 6 million children in the US, with 2.7 million African American children (Office of Minority Health, n.d.). In 2019, it was also reported by the Office of Minority Health that Black children were three times more likely to die from asthma and five times more likely to be hospitalized compared to their White counterparts.
Environmental Factors that Contribute to Asthma Development
According to Environmental Protection Agency (2017), the most common environmental factors that worsen asthma in children are air pollution, secondhand smoke, and mold, especially in minority-based rural and urban neighborhoods. Low-income housing poses greater risks through “increased moisture, mold, and insect exposure. Poor ventilation also opens allergens and other airborne toxins to suffocate the home, which can lead to fatal consequences” (Pacheco et al., 2014).
Mental and Physical Effects of Pediatric Asthma
Not only does pediatric asthma affect children physically, through coughing, wheezing, and chest tightness, but mentally as well. Approximately 50% of children who have asthma missed a day or more of school, contributing to the top three leading causes of school absenteeism in the United States (Hsu et al., 2016). Asthma may stunt intellectual and academic development through poor academic achievement from missed school days and increased dropout rates (Moonie et al., 2008). Children may also experience more anxiety, stress, depression, and behavioral issues from deficits in asthma control. Unmanaged asthma contributes to disruptions in sleep, physical activity, and social interactions with other children, especially if those children are exposed to triggers that cause asthma attacks (AAFA, 2018). However, if asthmatic symptoms are consistently controlled, children will face fewer asthma attacks and enjoy the activities they are wary of (Hsu et al., 2016).
How to Manage Pediatric Asthma
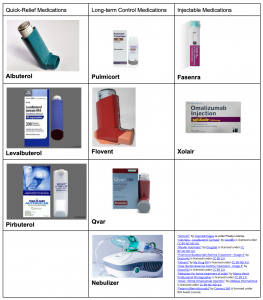
There are two medicine-based methods to manage pediatric asthma: quick-relief and long-term control medications. Quick-relief medications are usually bronchodilators accompanied by spacers to ensure the medicine completely enters the lungs and improve persistent asthma. Long-term control medications often include inhaled corticosteroids that do not immediately relieve flare-ups, but prevent chronic asthma attacks. Finally, injectable medications treat moderate-to-severe asthma subcutaneously on a monthly or bimonthly basis. If certain medicines are not readily available, breathing exercises are also useful in easing symptoms. The Global Allergy & Airways Patient Platform (GAAPP, 2021) describes the best breathing exercises to increase overall lung capacity and strength on its website.
Asthma Management in Schools
Asthma management in schools and households reduces the number of attacks in child asthmatics. All fifty states in the US have regulations in place that allow children to self-carry and administer their own asthma medication in school (AAN, 2022). The Student Readiness Tool allows parents and nurses (or other healthcare administrators if no nurses are present) to examine the student’s understanding of their asthma triggers, how to administer medication, and if they recognize the symptoms of an asthma attack before they carry inhalers independently. In all, asthma education and awareness between the family and staff can develop a healthy school and home environment. They can work together to offer safe physical education activities and create a suitable atmosphere for asthmatic children (American Lung Association, 2021).
Asthma Management at Home
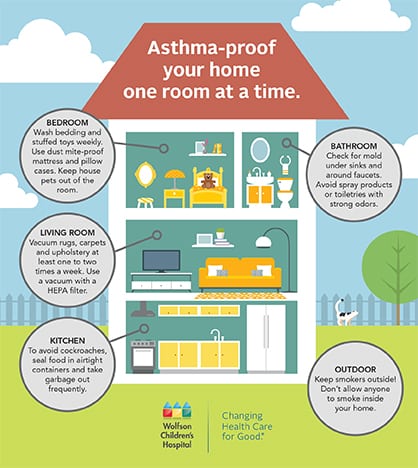
In households, properly shutting windows and doors to prevent pollen and poor air quality are essential during the spring and summer months. Preventive measures include frequently vacuuming and shampooing carpets to clear dust and pet dander, using unscented cleaners and sprays, and wearing a mask while cleaning to add protection for the child and prevent particles from blocking the airways (American Lung Association, 2020). Lastly, reducing asthma triggers, such as limiting smoking to prevent secondhand smoke and regularly changing linens, diminishes any external factors that aggravate symptoms (AAFA, 2015).
Action Plans
The most recognized way of managing pediatric asthma is enforcing action plans. Constant communication with the child’s allergist will provide the caregiver with recommendations and plans for treatment to keep the child’s asthma under control. Action plans allow them to track asthma symptoms, assess medication effectiveness, and record flare-ups. This data permits caregivers to modify and develop the best plan of action to regulate pediatric asthma before the child enters adulthood (Ben-Joseph, 2017). Working closely with school staff, specifically healthcare providers, coaches, and educators, at the child’s school to ensure they are aware of action plans authorizes them to navigate what to do should an asthma attack occur. Most importantly, caregivers should instruct children on what they need to do if a flare-up happens, they are exposed to triggers, or they forget their medicine. Caregivers are not always present, so instilling this is vital in making sure the child is proactive in their health (American College of Allergy, Asthma, and Immunology, n.d.).
Resources
The yearly medical cost per person with asthma is $3,266, including hospital costs, doctor’s visits, and prescriptions, which can be stressful for low-income families (Lebowitz & Arnold, 2020). Fortunately, federal-state programs (Medicaid and CHIP), community health centers, and both patient assistance programs (PAP) and co-pay assistance (CAP) programs provide financial aid for children and their families to cover medical expenses, asthma remedies, and cost-saving generic inhalers (Bass, 2020). Families usually have to pay more for remedy access due to high out-of-pocket costs, which increases the unaffordability rates of certain life-saving asthma treatments that several children require (AAFA, n.d.). By offering more inexpensive, generic alternatives that share the same purpose as brand medications, children can be the healthiest versions of themselves.
To learn more about ways to afford asthma treatment and medication, here are some helpful resources:
- GoodRx
- GoodRx is a CAP and PAP that provides free coupons and discount cards to use at participating pharmacies. GoodRx offers discounts for both brand and generic name prescriptions and is available for insured and uninsured individuals with up to 80% in savings.
- NeedyMeds
- NeedyMeds is a non-profit PAP that offers patient discount cards to use at participating pharmacies and can also be used for discounted lab tests and medical and dental services at health clinics. Though primarily intended for generic prescriptions, patients can save up to 80% on purchases. Scholarships are also available for students with medical difficulties to financially assist families with college tuition.
- GlaxoSmithKline (GSK)
- GSK is a PAP that offers 100% coverage for quick-relief medications. To qualify, patients cannot receive prescription drug benefits from insurance programs and must have an annual income 250% below the federal poverty line. GSK also includes a “dollars-off” program for individuals with commercial insurance on specific medicines, but the list is very limited.
- Merck
- Merck is a PAP that provides free coverage for oral, quick-relief, and nasal spray prescriptions that are intended for uninsured individuals. Similar to GSK, patients cannot receive drug benefits from public or private insurance and must have an annual income 400% below the federal poverty line. Merck also provides vaccines and replacement antidotes in hospitals.
Key Takeaways
- Pediatric asthma has both internal and external effects. Not only do symptoms include coughing, wheezing, and trouble breathing, but poorly managed asthma increases days missed in school, sleep disturbances, and limited participation in social activities.
- Important aspects of asthma treatment include short and long-term medication, education and awareness, avoiding triggers through routine cleaning, and establishing an action plan between the child, caregiver, and healthcare professional.
- There are countless local, state, and federal programs that offer low to no-cost medication, covered medical insurance, and alternatives that best fit the child’s individual needs.
References
Advocacy with Allergy & Asthma Network. (2022). State laws. https://advocacy.allergyasthmanetwork.org/laws-to-protect-those-with-allergies-and-asthma/state-laws/.
American Lung Association (2020). Healthy air at home. https://www.lung.org/clean-air/at-home.
American Lung Association. (2021). Back to school with asthma toolkit. https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/living-with-asthma/creating-asthma-friendly-environments/back-to-school-with-asthma-toolkit.
Asthma and Allergy Foundation of America. (2015). Control indoor allergens to improve indoor air quality. https://www.aafa.org/control-indoor-allergens/.
Asthma and Allergy Foundation of America. (2018). Strong emotions, stress and depression can trigger asthma. https://www.aafa.org/emotions-stress-depression.aspx.
Asthma and Allergy Foundation of America. (n.d.) Cost of asthma on society. https://www.aafa.org/cost-of-asthma-on-society/.
Bass, P. (2020). Prescription assistance programs for asthma drugs. Verywell Health. https://www.verywellhealth.com/patient-assistance-program-for-asthma-medication-200788.
Ben-Joseph, E.P. (2017). What’s an asthma action plan (for parents)? KidsHealth. https://kidshealth.org/en/parents/action-plan.html.
Environmental Protection Agency. (2017). Understanding how environmental factors affect children’s asthma. https://www.epa.gov/sciencematters/understanding-how-environmental-factors-affect-childrens-asthma#:~:text=%5B1%5D%20Environmental%20factors%20such%20as,can%20worsen%20common%20asthma%20symptoms.
Global Allergy & Airways Patient Platform. (2021). Breathing exercises and techniques for asthma. https://gaapp.org/asthma-treatment-and-medicines/breathing-exercises-techniques-for-asthma/.
Hsu, J., Qin, X., Beavers, S. F., & Mirabelli, M. C. (2016). Asthma-related school absenteeism, morbidity, and modifiable factors. American Journal of Preventive Medicine, 51(1), 23–32. https://doi.org/10.1016/j.amepre.2015.12.012.
Kibirige, D., Sanya, R.E., Nantanda, R., Worodria, W., & Kirenga, B. (2019). Availability and affordability of medicines and diagnostic tests recommended for management of asthma and chronic obstructive pulmonary disease in sub-Saharan Africa: a systematic review. Allergy Asthma Clin Immunol 15(14). https://doi.org/10.1186/s13223-019-0329-2.
Lebowitz, L. & Arnold, M. (2020). Financial assistance programs for asthma patients. Asthma.net. https://asthma.net/clinical/financial-assistance-programs.
Mayo Clinic. (2022). What to know about asthma treatment for kids ages 5 to 11. Mayo Foundation for Medical Education and Research. https://www.mayoclinic.org/diseases-conditions/childhood-asthma/in-depth/asthma-in-children/art-20044383.
Moonie, S., Sterling, D. A., Figgs, L. W., & Castro, M. (2008). The relationship between school absence, academic performance, and asthma status. Journal of School Health, 78(3), 140–148. https://doi.org/10.1111/j.1746-1561.2007.00276.x.
Office of Minority Health. (n.d.). Asthma and african americans. HHS.gov. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=15.
Pacheco, C. M., Ciaccio, C. E., Nazir, N., Daley, C. M., DiDonna, A., Choi, W. S., Barnes, C. S., & Rosenwasser, L. J. (2014). Homes of low-income minority families with asthmatic children have increased condition issues. Allergy and Asthma Proceedings, 35(6), 467–474. https://doi.org/10.2500/aap.2014.35.3792.
U.S. National Library of Medicine. (2021). Asthma in children | asthma symptoms. MedlinePlus. https://medlineplus.gov/asthmainchildren.html.
Veoli, A. (2018). Can students self-carry their asthma inhaler in schools? Asthma.net. https://asthma.net/living/can-students-self-carry-their-asthma-inhaler-in-schools.
Asthma caused by allergies.
Asthma caused by anything but allergies.
Asthma that worsens at night.
Asthma where the main symptom is a dry, continuous cough.
Asthma caused by irritants in the workplace.
Absence from work or school.
Inhaled asthma medication that expands the bronchi, or passages that carry air to and from the lungs.
A football-shaped empty tube that holds an inhaler in place and makes it easier for medicine to enter the lungs.
The most effective asthma medication that prevents inflammation and redness in the airway through inhaling medicine.
Under the skin.

