21 Childhood Anxiety and Depression
Lawson Logue
Introduction
Anxiety and depression are mental disorders that can be severe issues for any age group. A recent study found that around 7.1% of children aged 3-17 suffer from anxiety, and 3.2% suffer from depression (Reem et al., 2019). Mental illnesses in childhood can lead to adverse social, emotional, cognitive, and academic development. Anxiety is defined as a steady unease that can negatively affect thoughts, behaviors, or actions (Center for Disease Control and Prevention, 2021). Depression is defined as a constant feeling of sadness, irritability, or hopelessness that can negatively affect thoughts, behaviors, or activities (Center for Disease Control and Prevention, 2021). Since anxiety and depression among children are very common, caregivers need to be aware of the best ways to help an affected child cope with their mental illness.
Types, signs, and symptoms
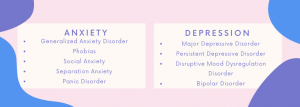
Many types of anxiety and depression affect children. The most common types of anxiety (Anxiety and Depression Association of America, 2015) and depression (DiMaria, 2020) in children are listed below.
Caregivers can find general signs and symptoms of both anxiety and depression in children in this CDC article. While these signs and symptoms give a brief overview of the different mental illnesses, it is essential to note that anxiety and depression differ from child to child based on age groups, the different types of mental diseases, and external factors affecting the child (Center for Disease Control and Prevention, 2021). If caregivers see these signs or symptoms in children, it is essential to intervene and seek help. The specific steps and resources a caregiver can use are in the last sections of this chapter.
Causes of Anxiety in Children and Teenagers
Triggers for anxiety often occur in childhood or during adolescence (Dabkowska & Dabkowska-Mika, 2015). One cause of anxiety in children includes specific life situations. These events lead to increased feelings of fear, uneasiness, or worry. Examples include divorce, serious illness, death of a loved one, or abuse. Each situation leads to stress and changes in development (Dabkowska & Dabkowska-Mika, 2015).
Another cause of anxiety in children is learned behaviors. Learned behaviors are anything that a parent teaches, intentionally or unintentionally, to a child (Aktar et al., 2017). Parents can pass down fears to their children in nonverbal or verbal ways. Children often learn from their parents by observing their behaviors, especially in the first few years. If a parent gives an anxious or fearful reaction to a specific event, the child will likely learn this behavior (Aktar et al., 2017).
Anxiety has been linked to heredity. If at least one parent has an anxiety disorder, their children have an increased risk of an anxiety disorder (Dabkowska & Dabkowska-Mika, 2015). Even if a child has this genetic factor, he or she is not guaranteed to develop anxiety. Still, it puts them at a higher risk of developing anxiety if exposed to other anxiety-causing elements (Dabkowska & Dabkowska-Mika, 2015).
Causes of Depression in Children and Teenagers

Like childhood anxiety, many different risk factors can lead to childhood depression. Everyday life situations that often lead to depression include bullying, stressful events, and physical health (Holland, 2019). Bullying is one of the leading causes of childhood depression because of its emotional effects (Winding et al., 2020). Bullying can lead to withdrawing from family and friends, behavioral issues, self-esteem issues, and long-term mental health issues (Holland, 2019).
Stressful events are linked to childhood depression. Long-term stressful events can lead to harmful effects on a child’s development and specific brain chemistry, leading to depression. Long-term stressful events include abuse, divorce, racism, and changes in school life or home life (Levinson & Nichols, n.d.).
Physical health can lead to depression in children, especially in chronic illnesses. With chronic diseases, like autoimmune diseases or cancer, it is common for the child to feel hopeless and alone. There are also genetic linkages to childhood depression. Depression has a 50% chance the condition runs in the family (Levinson & Nichols, n.d.). Similar to anxiety, depression is not guaranteed to develop in children who have a genetic component, but there is an increased risk of developing the mental illness based on how many depression-causing elements the child is exposed to (Dabkowska & Dabkowska-Mika, 2015).
How to Help A Child with Anxiety or Depression
Once signs and symptoms of depression or anxiety are recognized, caregivers can assist with seeking treatment options. First, they should be supportive and try to talk with the child. Then, caregivers can discuss with their primary care doctor to determine the next steps. The doctor will examine the child for physical and mental signs and, if necessary, refers to a therapist or psychiatrist for medication and/or cognitive-behavioral therapy (Center for Disease Control and Prevention, 2021). The best course of treatment depends on the child’s needs.
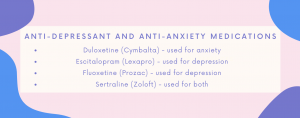
Once a child is referred to a psychiatrist, they will be evaluated with specialized tests to determine mental illness severity. If medication is needed, a child will be prescribed an anti-depressant or anti-anxiety to lessen their symptoms. The most common types prescribed to children can be seen in the chart below (Mayo Clinic Staff, 2022).
While drugs may help, treatment success increases when paired with talk therapy. If a child is referred to a therapist or a psychiatrist, then they will receive cognitive-behavioral therapy (CBT). CBT is the most commonly used treatment for anxiety and depression (Center for Disease Control and Prevention, 2021). This type of therapy focuses on how thoughts and emotions affect behaviors in combination with learning how to divert negative behaviors to minimize stressful situations (Pietrangelo, 2019). In CBT, the child, caregiver, and therapist work together to make goals and a strict treatment plan. The most common techniques that cognitive-behavioral therapy use include play therapy, modeling, restructuring, and exposure (Pietrangelo, 2019). Play therapy uses role-playing to help address problems and work through solutions. Modeling also uses role-playing, where the therapist teaches methods to divert situations. Restructuring allows the child to learn to change negative behavior into a better one. Finally, exposure includes the therapist slowly showing the child situations that trigger anxiety or depression (Pietrangelo, 2019).
Resources
Childhood anxiety and depression can be difficult for a parent to understand if they have not experienced these mental health conditions before. See the resources below to further help children with their anxiety and/or depression.
- National Institute of Mental Health
- The National Institute of Mental Health gives an excellent overview of child and adolescent mental health. It details the warning signs of both young children and older children/adolescents from a broader view of mental health. This website also gives multiple helplines that might be useful for children struggling with anxiety, depression, or other mental health issues to save on their phones.
- The Child Mind Institute
- The Child Mind Institute gives a deeper dive into anxiety, specifically for caregivers. It provides advice on parenting anxious children and how to help an anxious child in school. The website offers ways to aid specific nervous behaviors, like sleepover anxiety and testing anxiety.
- MentalHealth.gov
- This website provides multiple options on how to get help with mental health. It gives direct links on getting immediate help, finding treatment options near you, support for veterans and their families, information on health insurance and mental health options, and ways to get started in clinical trials.
Key Takeaways
- Anxiety and depression are serious issues when it comes to the adequate development of children.
- Symptoms of anxiety in children include persistent worrying, irritability, and fear of normal activities.
- Symptoms of depression in children include persistent sadness, not wanting to participate in things they used to enjoy, and showing self-destructive or self-harming behaviors.
- There are multiple causes of both anxiety and depression, including genetic factors, life situations, and learned behaviors.
- If caregivers are concerned about their child having anxiety or depression, it is vital to seek additional help from a doctor, mental health specialist, or other healthcare professionals.
- Treatment usually consists of medication and/or talk therapy, commonly referred to as cognitive-behavioral therapy. When treating childhood anxiety and depression, it is essential to find a treatment plan and stick to it. Treating anxiety and depression early creates better childhood development outcomes.
References
Aktar, E., Nikolic, M., & Bogels, S. M. (2017). Environmental transmission of generalized anxiety disorder from parents to children: worries, experiential avoidance, and intolerance of uncertainty. Dialogues in Clinical Neuroscience, 19(2), 137-147. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5573558/
Anxiety and Depression Association of America. (2015, September). Childhood anxiety disorders. https://adaa.org/find-help/by-demographics/children/childhood-anxiety-disorders
Center for Disease Control and Prevention. (2021, March 21). Anxiety and depression in children. https://www.cdc.gov/childrensmentalhealth/depression.html
Dabkowska, M., & Dabkowska-Mika, A. (2015). Risk factors of anxiety disorders in children. In F. Durbano (Ed.), A Fresh Look at Anxiety Disorders. IntechOpen. https://www.intechopen.com/chapters/48919
DiMaria, L. (2020, March 8). Depressive disorders in children: symptoms, risk factors, diagnosis, treatment, and coping. Verywell Mind. https://www.verywellmind.com/depressive-disorders-in-children-1066782
Holland, K. (2019, February 21). Childhood depression: how to help your child. Healthline. https://www.healthline.com/health/mental-health/childhood-depression#symptoms
Levinson, D. F., & Nichols, W. E. (n.d.). Major depression and genetics. Stanford Medicine. https://med.stanford.edu/depressiongenetics/mddandgenes.html
Mayo Clinic Staff. (2022, February 26). Antidepressants for children and teens. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/teen-depression/in-depth/antidepressants/art-20047502
Pietrangelo, A. (2019, December 5). Cognitive-behavioral therapy (CBT) for kids: how it works. Healthline. https://www.healthline.com/health/mental-health/cbt-for-kids
Reem, G. M., Sherman, L. J., Vladutiu, C. J., Lynch, S. E., Bitsko, R. H., & Blumberg, S. J. (2019, March 1). Prevalence and treatment of depression, anxiety, and conduct problems in US children. The Journal of Pediatrics, 206(3), 256-267. https://www.jpeds.com/article/S0022-3476(18)31292-7/fulltext#relatedArticles
Winding, T.N., Skouenborg, L.A., Mortensen, V.L., & Andersen, J.H. (2020, November 19). Is bullying in adolescence associated with the development of depressive symptoms in adulthood?: A longitudinal cohort study. BMC Psychology, 8. https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-020-00491-5#citeas
an individual specializing in the therapeutic medical treatment of impairment, injury, disease, or disorder
a physician who practices psychiatry.
psychotherapy that combines cognitive therapy with behavior therapy by identifying faulty or maladaptive patterns of thinking, emotional response, or behavior and substituting them with desirable patterns of thinking, emotional response, or behavior —abbreviation CBT
psychotherapy in which a child is encouraged to reveal feelings and conflicts in play rather than by verbalization
therapy in which a particular behavior is elicited by the observation of similar behavior in others.
to effect a fundamental change in.
the act of exposing, laying open, or uncovering.

