5 Teenage Pregnancy
Emma Booth
Introduction
More recently, the United States has seen a decline in the overall rate of teenage pregnancy, but the United States still has one of the highest rates in the world (Centers for Disease Control and Prevention [CDC], 2021). The American Pregnancy Association (2021) defines teen pregnancy as “any pregnancy that occurs for a woman under the age of 20”. Having a child this young can put both the mother and baby in a high-risk position. The risks range from medical to financial, as well as social consequences. While there are challenges, many resources are available to help these young mothers and their babies.
Effects on the Young Mother

Many mothers do not recognize the consequences of giving birth at a young age until after they have occurred. Medical problems include a higher risk of preeclampsia, hypertension, depression, infection, low intake of vitamins and minerals, and anemia (American Pregnancy Association, 2021). These conditions increase the need for proper prenatal care, adding to the cost of the pregnancy. The financial burden of having a child is another concern because it adds another mouth to feed. Many teens who become pregnant do not have a chance to finish school, or they choose to drop out. A lack of education makes it harder for them to get a job and leads to a lower income (World Health Organization [WHO], 2020). More specifically, 30% of girls who dropout of high school mention parenthood as a reason (Shuger, n.d). Fortunately, several resources are available to allow a young mother to continue her education while becoming a parent, which will be discussed later in this chapter.
According to the World Health Organization (2020), there are also effects on the mother’s social well-being. They may face rejection from friends and family and will have less time to spend with peers because of greater responsibilities at home. Young mothers may start to feel isolated and lonely as their responsibilities increase. Mothers who experience domestic violence have additional mental and emotional health damage (WHO, 2020).
Effects on the Child
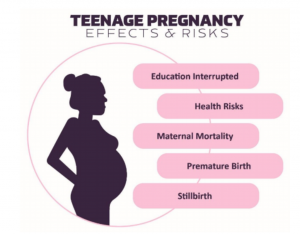
A child is at risk for several other events if they have a younger mother. The baby is more likely to be born prematurely, have a low birth weight, and have medical complications (American Pregnancy Association, 2021). Complications that may arise are sudden infant death syndrome and birth defects (D’Alessandro, 2007). If the mother struggles, the child can experience social challenges such as lower academic achievement, lack of emotional support, behavioral issues, and fewer social skills (Youth.gov, n.d.). The child will also have to bear the challenges of the mother’s low educational and financial achievements, leading to a reliance on public funds (Youth.gov, n.d).
Resources
Teenage mothers and their children may feel as though they have to go through this alone, but this is not the case. Family, friends, and doctors are great resources to go to for support. Most importantly, teen mothers need to regularly visit a doctor during and after pregnancy. This ensures the mother is partaking in proper prenatal care, which includes the healthcare received during pregnancy. This includes having proper nutrition, exercising, getting a good amount of sleep, avoiding alcohol and drugs, and receiving education from their doctor (Ben-Joseph, 2017). During pregnancy, the doctor monitors the baby and the mother’s health as the pregnancy progresses. The child’s pediatrician is helpful in making sure the baby is reaching the proper milestones and can address any medical issues that may arise, as well as confirm the teen has access to transportation, food, housing, insurance, etc. (Powers et al., 2021).
Doctors can also ensure the mother and baby are receiving proper support in their community by introducing them to specific resources. In the U.S., many government and private organization resources are available to assist both the mother and child to live a long and healthy life. Below are several resources available to young mothers during this challenging time:
- Temporary Assistance for Needy Families (TANF)
- A government funded grant that gives states money to assist low-income families with children. TANF hopes to promote a stable home life and provide greater access to food, transportation and childcare (Office of Family Assistance, 2019).
- Second Chance Homes
- This program gives teens who experience negative situations at home (ex., abuse and neglect) a place to move for their safety and their baby. The homes are group homes or apartments supervised by an adult. The homes provide a stable environment for the teen to become independent while also providing childcare and encouraging high school completion (U.S. Department of Housing and Urban Development, n.d.).
- Children’s Health Insurance Program (CHIP)
- A government program that currently provides health insurance to 9.6 million children whose families do not qualify for Medicaid, but are unable to afford private health insurance. It is available for individuals up to the age of 19; therefore, both mother and baby can qualify (Chen & Gibson, 2022).
- Planned Parenthood
- Planned Parenthood is a non-profit organization that provides free healthcare, supplies and education about pregnancy to individuals in the community. Expectant mothers can go to their website to locate a clinic near them where they can utilize social and medical support.
Key Takeaways
- Teenage pregnancy can have adverse social, financial, and physical outcomes on the young mother.
- The baby is also at risk for negative outcomes regarding their physical and developmental health.
- Mothers should utilize the resources available to help them throughout their pregnancy and after the baby is born.
- Government resources are available, such as TANF, CHIP, and Second Chance Homes, as well as non-profit organizations.
- Asking for help will make the experience less stressful for both the new mother and the child, reducing the negative effects on the child and mother.
References
American Pregnancy Association. (2021). Teenage pregnancy. https://americanpregnancy.org/unplanned-pregnancy/teenage-pregnancy/
Ben-Joseph, E.P. (2017). Having a healthy pregnancy (for teens). https://kidshealth.org/en/teens/pregnancy.html
Centers for Disease Control and Prevention. (2021). About teen pregnancy. https://www.cdc.gov/teenpregnancy/about/index.htm
Centers for Medicare & Medicaid Services. (n.d). Children’s health insurance program. https://www.medicaid.gov/chip/index.html
Chen, A. & Gibson, C. (2022). CHIP provides critical reproductive health care to adolescents and pregnant women. https://healthlaw.org/chip-provides-critical-reproductive-health-care-to-adolescents-and-pregnant-women/
D’Alessandro, D. (2007). What are some of the complications of teen pregnancy? https://pediatriceducation.org/2007/04/09/what-are-some-of-the-complications-of-teenage-pregnancy/
Office of Family Assistance. (2019). About tanf. https://www.acf.hhs.gov/ofa/programs/tanf/about
Powers, M.E., Takagishi, J. & Committee on Adolescence, Council on Early Childhood. (2021). Care of adolescent parents and their children. Pediatrics, 147 (5), 1-15. https://doi.org/10.1542/peds.2021-050919
Shuger, L. (n.d). Teen pregnancy and high school dropout. https://www.americaspromise.org/sites/default/files/d8/legacy/bodyfiles/teen-pregnancy-and-hs-dropout-print.pdf
U.S. Department of Housing and Urban Development. (n.d.). About second chance homes. https://www.hud.gov/program_offices/public_indian_housing/other/sch/about#5
World Health Organization. (2020, January 31). Adolescent pregnancy. https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy
Youth.gov. (n.d). The adverse effects of teen pregnancy. https://youth.gov/youth-topics/pregnancy-prevention/adverse-effects-teen-pregnancy
a serious condition developing in late pregnancy that is characterized by a sudden rise in blood pressure, excessive weight gain, generalized edema, proteinuria, severe headache, and visual disturbances and that may result in eclampsia if untreated
abnormally high blood pressure and especially arterial blood pressure
a condition in which the blood is deficient in red blood cells, in hemoglobin, or in total volume
death of an apparently healthy infant usually before one year of age that is of unknown cause and occurs especially during sleep

