12 Stress and Anxiety
John Williams
Stress and anxiety is the number one mental health disorder for men in America (Infographic: Mental health for men). Anxiety disorder is defined as persistent anxiety that does not go away and interrupts daily life (Anxiety Disorders). Approximately 19.1 million American men ages 18-54 have some sort of anxiety disorder (Infographic: Mental health for men). As of recent, mental health awareness has exploded and has become a point of emphasis as societal opinions on the topic has shifted from intolerance to support. However, many men still find themselves unable to speak on the matter. Evidence shows that 77% of men have experienced negative mental health symptoms, but 40% of men have not spoken about their issues (40% of men won’t talk to anyone about their mental health). Ranked at the number one mental disorder in terms of prevalence, anxiety disorder causes the most issues for men in terms of their mental health. From a Public Health point of view, anxiety disorder is highly treatable (Bandelow et al., 2017). Therefore, finding solutions to increase the treatment rate is key to eliminating this disorder. However, in the United Kingdom, a cross-sectional survey found that it would require suicidal thoughts or self-harm to get them to see a mental health professional (40% of men won’t talk to anyone about their mental health). The resistance to medical treatment for mental health is created through social stigmas and norms that have been cultivated through the decades. In this past century, much has changed about how men interact with the world around them. However, the social norms surrounding their interaction have remained mostly unchanged. This can be seen clearly in the social norms surrounding men’s utilization of mental healthcare. Masculine social norms encompass the filling a specific role in the social unit such as the masculine provider mentality. This is a common trait exhibited by American males that often puts males as the sole provider for a family unit (Brown, 2021). This role puts large pressures on the male to provide, creating stress and anxiety among males financially. This means masculine roles contribute to increasing anxiety and stress among men.

“Anxiety” by Nick Youngson is licensed under CC BY-SA 3.0
How Do These Factors Work?
Financial Stability
Financial instability and discomfort are areas often identified as a major trigger for men and anxiety disorders. Financial instability can be the precursor to mental and physical health problems such as the previously mentioned anxiety, stress, hypertension, and heart disease (Pogosova et al., 2021). However, financial instability just acts as a powerful stressor for men, and over time this stress creates anxiety and then anxiety disorders in men when they are financially unstable (Sareen, 2011). Therefore, we can connect men’s financial instability to bad health outcomes through anxiety disorders by further identifying how anxiety links to poor health outcomes. Looking at a comprehensive study done for half-of-a-million adults found that coronary heart disease and anxiety or anxiety disorders were positively correlated (Wu et al., 2022). Furthermore, the link between anxiety and low socioeconomic status was confirmed in a study published by Elsevier/North-Holland Biomedical Press, where low income and low socioeconomic status was highly correlated with anxiety (Nunes et al., 2022). A Priory Group’s cross-sectional survey of 1000 men in the United Kingdom gives us insight into this factor. These men outlined their largest causes for their mental health problems, and the study identified that the second most prevalent cause of negative mental health issues with men is financial issues at 31%, just behind work pressures at 32% (40% of men won’t talk to anyone about their mental health). While this study does not analyze American men, it gives us insight into how stresses affect men on a more general scale. These two major causes for negative mental health in men are connected through employment, showing that men and their jobs cause a combined 63% of mental distress.
Racialized Experiences Among Students
The notion that social or political inequalities for minorities cause anxiety and poor mental health outcomes for racial minorities is not a new idea. In a recent study conducted among undergraduate students, it was found that minority stress from microaggressions and discrimination was related to students’ status as racial minorities, meaning that their race created the anxiety symptoms they experienced (Manzo et al., 2022). We can infer from these findings that current minority members find themselves at a higher risk factor for anxiety than non-minority members in 2022. The relationship between a student’s racial or ethnic background and anxiety symptoms are explained by the authors through the lens of Minority Stress Theory or MST. MST is a theoretical framework that aims to understand how microaggressions, discrimination, or prejudice create disparities between minorities mental health outcomes and non-minority mental health outcomes though the constant taxation of a minorities coping mechanisms. We can infer from these findings that minority populations may find themselves at a higher risk factor for anxiety than white populations.
Racialized Experiences Among Employees
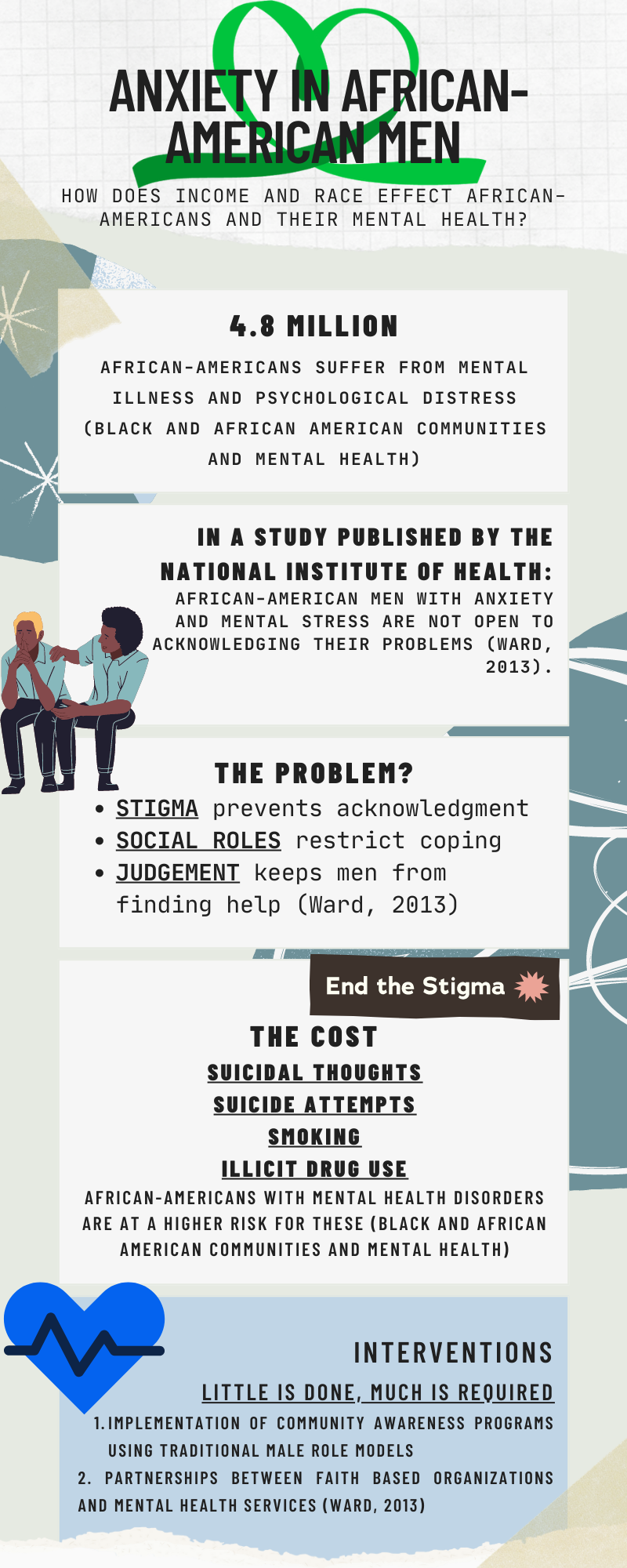
Moving away from students and looking into the African American community, we see similar results. Poor African American men who are financially unstable due to unemployment may find themselves with increased anxiety on two levels. The first level being stress resulting from not paying the bills, and the second level being unable to fulfill the breadwinner social role that men perceive as their duty due to societal norms (Robinson et al., 2021). The perceived failure to adhere to the societally dominant ideas of manhood have more negative effects than being low income. This intimates a deeper struggle to men than just wealth and race. The connection shows that the lack of money creates an inability to fill male gender roles, creating psychological disparity among low income and minority males. Suggesting that employment status is leading to a situation where the male is generating massive amounts of anxiety over the cognitive dissonance experienced by the confliction of their social role and current role. Additionally, the male gender roles of perseverance and grit mask the symptoms of anxiety and stress, further reducing one’s ability to recognize anxiety disorders (Fisher et al., 2022). Those studied also made their employment status as employed or unemployed connected to their self-esteem as a man and a contributing member of their race. This create a heightened experience of anxiety that may lead to other mental challenges like depression and suicide.

“Man Stressed At Work Illustration” by Ciphr Connect is licensed under CC BY 2.0
The Intersection Between Race and Income
Refugees
There are various forms of racial inequality that can be formed at different populations. Refugees are an interesting population to examine as they can inherently be both at an income and racial disparity just through their existence as refugees in a foreign state. Researchers identified minority refugees, or non-white refugees, in high-income countries and surveyed their anxiety levels. Researchers found that 42% of refugees reported anxiety, which is outlined as substantially higher than those who lived in non-refugee populations or those living in a war or conflict zone (Henkelmann et al,. 2020). This study found astonishing results as to the elevated risk of anxiety at the intersection of income and race. Anxiety levels were much higher than comparable populations of minorities as well as populations that would be considered in high stress situations such as those outlined living in warzones. While the study was not conducted on men, the data found shows that in a population in which income and race are at a disparity, we see extreme stress. Similarly, through this study, we can clearly identify the drastic compounding effect that each of these factors have on anxiety.
Relieving the Pressure: Public Health Interventions
Current Public Health Interventions
The successful and efficient implementation of an intervention is the most difficult part of fixing a public health crisis. There are very few active public health interventions to address and prevent anxiety disorders and stress in men caused by income and race. There are several treatments and interventions used to treat anxiety and anxiety disorders as they arise. One treatment for anxiety disorder is psychotherapy. Psychotherapy is known as talk therapy as it uses a psychologist to talk through anxiety inducing situations. The gold standard of psychotherapy is cognitive behavioral therapy. CBT as it is known teaches patients to think and react differently to situations that would normally cause them anxiety. However, this follows a traditional path for disease treatment in the american healthcare system, meaning that this method only continues to treat the disease and not focus on its prevention. But without any form of treatment for men that prevents anxiety or stress related negative mental health outcomes, these interventions will do little to fix any problems American men face. Overall, with the lack of implemented interventions, we can only propose what could be done to correct this public health crisis.
Struggles Identifying Anxiety and What It Means For Suicide
Anxiety and stress are expressed differently among men. Due to the individual nature of mental health, each man facing stress and anxiety will respond differently. This becomes even more complex at the intersection of race. People of racially and culturally diverse backgrounds each express stress and anxiety differently given their adopted norms (Fisher et al., 2022). On top of this, cultural norms can also affect one’s willingness to see a mental health doctor, further creating problems for men’s treatment of anxiety and stress. This key inefficiency among highlighting anxiety and stress symptoms has made these mental health disorders a unique risk factor is male suicide (Fisher et al., 2022). There is little consideration of anxiety and stress in American as well as global suicide prevention, and understanding how anxiety disorder affects men and suicide could reduce suicide attempts in men across the country.
Recommendations
Starting by correcting this issue of race-based stress and anxiety. There have been studies created documenting stress and anxiety caused by discrimination in the African American population. A study published in The Journal of Racial and Ethnic Health Disparities showed a “strong” relationship between mistreatment due to race and levels of stress and anxiety (Williams et al., 2018). Research like this shows the need for support that minority men need to overcome and cope with current racial anxieties. With this in mind, I recommended an intervention strategy to improve the mental health outcomes of minority men who have been affected by racial anxiety and stress would be to create an intervention in the interpersonal and organizational levels of the ecological model of health. At the organizational level, an intervention to target race-based anxiety would be to create a program through the Men’s Mental Health Network that serves the minority community through counseling, group therapy, advocating for the community, awareness, and through connecting the community to medical resources to aid their anxieties and stresses.
At the interpersonal level, improving the utilization of healthcare services among men through targeted awareness campaigns to normalize mental health issues and to reduce the stigma surrounding men and mental healthcare. A study published by the American Journal of Men’s Health recommended interventions that would improve male help-seeking by incorporating the use of role models, motivating men to change the social norm to not see doctors for mental health crisis, and symptom management and recognition (Sagar-Ouriaghli et al., 2019). We would recommend a similar solution to change the social stigma of men and mental healthcare utilization through normalizing it. This can be done through targeted ads online or on television by using popular and traditional male role models such as professional athletes. An example of nne of these ads is “The Power of Okay” campaign by See Me. See Me is a Scottish based national mental health program dedicated to ending discrimination and mental health stigmas. The campaign targeted the Scottish workforce, asking people to check up on their peers (Power of Okay). This was in response to a survey that See Me conducted that showed that 48% of employees have anxiety of losing their jobs. While this is not an American based program, it shows the need for these campaigns in the workplace and in other places of the world.
Key Takeaways
- Income instability and race are factors that are both associated with anxiety disorders and stress in men. Additionally, income instability and race are risk factors for poor physical health outcomes such as hypertension and heart disease.
- For men, masculinity plays a large role in the anxiety and stress related response of men due to the social norm of being providers, workers, and breadwinners.
- Interventions for tackling anxiety disorders and stress caused by income inequality and race are not currently in effect. However, there are several programs attempting to help ease the stigma of men and mental healthcare utilization.
Chapter Review Questions
- Stress and Anxiety are precursors to which of the following physical health outcomes?
- A. Arthritis
- B. Hypertension
- C. Bipolar Disorder
- D. Carpal Tunnel Syndrome
- In a study by The Journal of Racial and Ethnic Health Disparities, what did they publish about race-based anxiety?
- A. Anxiety and stress are linked to genetics more so than experiences
- B. Discrimination is weak factor in race-based anxiety of African Americans
- C. That there was no correlation between discrimination and race-based anxiety
- D. Discrimination is a strong factor in race-based anxiety of African Americans
- What is the relationship between unemployment and anxiety in men?
- A. Men’s anxiety is increased due to unemployment
- B. Men experience no change in their anxiety levels due to their employment status
- C. Men’s anxiety is increased more when they are employed than when they are unemployed
- D. Men’s anxiety is decreased when they are unemployed
- How does masculinity effect a Man’s stress and anxiety level when faced with unemployment?
- A. Their social (masculine) role becomes conflicted with their current role, causing mental stress
- B. The man alters his social role to become more like his current role and experience little to no stress
- C. Masculinity has no effect on anxiety levels and unemployment
- D. None of the above
References
Anxiety and Depression Association of America. (2022, September 27). Anxiety Disorders – Facts & Statistics. ADAA. Retrieved October 5, 2022, from https://adaa.org/understanding-anxiety/facts-statistics
Bandelow, B., Michaelis, S., & Wedekind, D. (2017). Treatment of anxiety disorders. Dialogues in clinical neuroscience, 19(2), 93–107. https://doi.org/10.31887/DCNS.2017.19.2/bbandelow
Brown, B. (2021, October 16). The provider role indicates that masculinity is prosocial. The Centre for Male Psychology. Retrieved November 23, 2022, from https://www.centreformalepsychology.com/male-psychology-magazine-listings/the-provider-role-indicates-that-masculinity-is-prosocial#:~:text=Male%20provisioning%20stimulates%20paternal%20attachment,a%20father%20in%20the%20home.
Fisher, K., Seidler, Z. E., King, K., Oliffe, J. L., Robertson, S., & Rice, S. M. (2022). Men’s anxiety, why it matters, and what is needed to limit its risk for male suicide. Discover Psychology, 2(1), 18. https://doi.org/10.1007/s44202-022-00035-5
Henkelmann, J. R., de Best, S., Deckers, C., Jensen, K., Shahab, M., Elzinga, B., & Molendijk, M. (2020). Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: systematic review and meta-analysis. BJPsych open, 6(4), e68. https://doi.org/10.1192/bjo.2020.54
Manzo, G., Piña-Watson, B., & Kim, S. Y. (2022). Minority stress and academic outcomes among ethnic minority college students: Anxiety as a mediating mechanism. Journal of American College Health : J of ACH, 1–8. https://doi-org.libproxy.clemson.edu/10.1080/07448481.2022.2128683
Mental Health America. (n.d.). Black and African American communities and Mental Health. Mental Health America. Retrieved December 6, 2022, from https://www.mhanational.org/issues/black-and-african-american-communities-and-mental-health
Mental Health America. (n.d.). Infographic: Mental health for men. Mental Health America. Retrieved October 5, 2022, from https://www.mhanational.org/infographic-mental-health-men
Nunes, J. C., Carroll, M. K., Mahaffey, K. W., Califf, R. M., Doraiswamy, P. M., Short, S., Shah, S. H., Swope, S., Williams, D., Hernandez, A. F., & Hong, D. S. (2022). General Anxiety Disorder-7 Questionnaire as a marker of low socioeconomic status and inequity. Journal of Affective Disorders, 317, 287–297. https://doi-org.libproxy.clemson.edu/10.1016/j.jad.2022.08.085
Pogosova, N., Boytsov, S., De Bacquer, D., Sokolova, O., Ausheva, A., Kursakov, A., & Saner, H. (2021). Factors Associated with Anxiety and Depressive Symptoms in 2775 Patients with Arterial Hypertension and Coronary Heart Disease: Results from the COMETA Multicenter Study. Global Heart, 16(1), 73. https://doi-org.libproxy.clemson.edu/10.5334/gh.1017
Priory. (n.d.). 40% of men won’t talk to anyone about their mental health. Priory. Retrieved October 3, 2022, from https://www.priorygroup.com/blog/40-of-men-wont-talk-to-anyone-about-their-mental-health
Robinson, D., Valdez, L., Scott, L., & Buchanan, D. (2021). The role of work in gender identity, stress and health in low-income, middle-aged African-American men. Health promotion international, 36(5), 1231–1242. https://doi.org/10.1093/heapro/daaa144
Sagar-Ouriaghli, I., Godfrey, E., Bridge, L., Meade, L., & Brown, J. (2019). Improving Mental Health Service Utilization Among Men: A Systematic Review and Synthesis of Behavior Change Techniques Within Interventions Targeting Help-Seeking. American journal of men’s health, 13(3), 1557988319857009. https://doi.org/10.1177/1557988319857009
Sareen, J. (2011, April 4). Relationship between household income and mental disorders: Findings from a population-based longitudinal study. Archives of General Psychiatry. Retrieved October 31, 2022, from https://jamanetwork.com/journals/jamapsychiatry/fullarticle/211213
See Me. (n.d.). Power of Okay. See Me Scotland. Retrieved November 30, 2022, from https://www.seemescotland.org/seeus/campaigns/power-of-okay/#:~:text=The%20’Power%20of%20Okay’%20is,about%20mental%20health%20at%20work
Timmins, L., Schneider, J. A., Chen, Y.-T., Pagkas-Bather, J., Kim, B., Moody, R. L., Al-Ajlouni, Y. A., Lee, F., Koli, K., Durrell, M., Eavou, R., Hanson, H., Park, S. H., & Duncan, D. T. (2022). COVID-19 stressors and symptoms of depression and anxiety among Black cisgender sexual minority men and Black transgender women during the initial peak of the COVID-19 pandemic. Social Psychiatry and Psychiatric Epidemiology, 57(10), 1999–2011. https://doi-org.libproxy.clemson.edu/10.1007/s00127-022-02282-2
U.S. Department of Health and Human Services. (n.d.). Anxiety disorders. National Institute of Mental Health. Retrieved November 27, 2022, from https://www.nimh.nih.gov/health/topics/anxiety-disorders
U.S. Department of Health and Human Services. (n.d.). Any anxiety disorder. National Institute of Mental Health. Retrieved November 3, 2022, from https://www.nimh.nih.gov/health/statistics/any-anxiety-disorder
Ward, E. C., Wiltshire, J. C., Detry, M. A., & Brown, R. L. (2013). African American men and women’s attitude toward mental illness, perceptions of stigma, and preferred coping behaviors. Nursing research, 62(3), 185–194. https://doi.org/10.1097/NNR.0b013e31827bf533
Williams, M.T., Kanter, J.W. & Ching, T.H.W. (2018). Anxiety, Stress, and Trauma Symptoms in African Americans: Negative Affectivity Does Not Explain the Relationship between Microaggressions and Psychopathology. J. Racial and Ethnic Health Disparities 5, 919–927. https://doi.org/10.1007/s40615-017-0440-3
Wu, M., Zhu, Y., Lv, J., Guo, Y., Yang, L., Chen, Y., Tang, W., Xiang, S., Sun, X., Chen, J., Chen, Z., Yu, C., & Li, L. (2022). Association of anxiety with cardiovascular disease in a Chinese cohort of 0.5 million adults. Journal of Affective Disorders, 315, 291–296. https://doi-org.libproxy.clemson.edu/10.1016/j.jad.2022.08.008

