17 Substance Abuse in Rural Communities
Jake Baranoski
Substance abuse is a term used to describe the excessive use of drugs, both legal and illegal, that causes harmful effects on the user (John Hopkins, 2019). Substance abuse affects millions of people per year; social pressures, individual characteristics, and environmental factors play an important role in developing substance use disorders (John Hopkins, 2019). Each person has a different susceptibility to substance abuse, but people who have a mental health disorder and a history of addiction within their family are at higher risk to begin abusing substances (Mayo Clinic, n.d.). A factor that greatly affects substance abuse prevalence is whether or not the drugs are addictive. Stimulants or opioids can lead to addiction much faster than other drugs (Mayo Clinic, n.d.). Substance abuse can have several harmful effects on the user’s physical, emotional, spiritual, and social well-being. Those who abuse drugs often have at least one associated health issue, such as mental conditions, cancer, or heart disease (National Institute on Drug Abuse [NIDA], 2022). Substance abuse can impact a person’s ability to find and maintain a job, increase the likelihood of involvement in criminal activity, and damage their financial stability (Ignaszewski, 2021). At the community level, substance abuse rates have been linked to poverty, income inequality, and higher rates of violence (Ignaszewski, 2021).
Substance abuse can be treated through counseling, medications, and other medical devices to help with withdrawal (NIDA, 2019). It is essential to have regular follow-ups in the treatment plan to ensure relapse does not occur, if applicable (NIDA, 2019). Prevention of substance abuse is essential in protecting individuals and communities. Prevention programs are frequently used to target young populations before they begin using drugs. They aim to reduce risk factors and typically take place in community-level settings, such as schools, community centers, churches, or clubs (NIDA, 2020). While substance abuse affects diverse populations, men are typically at higher risk.
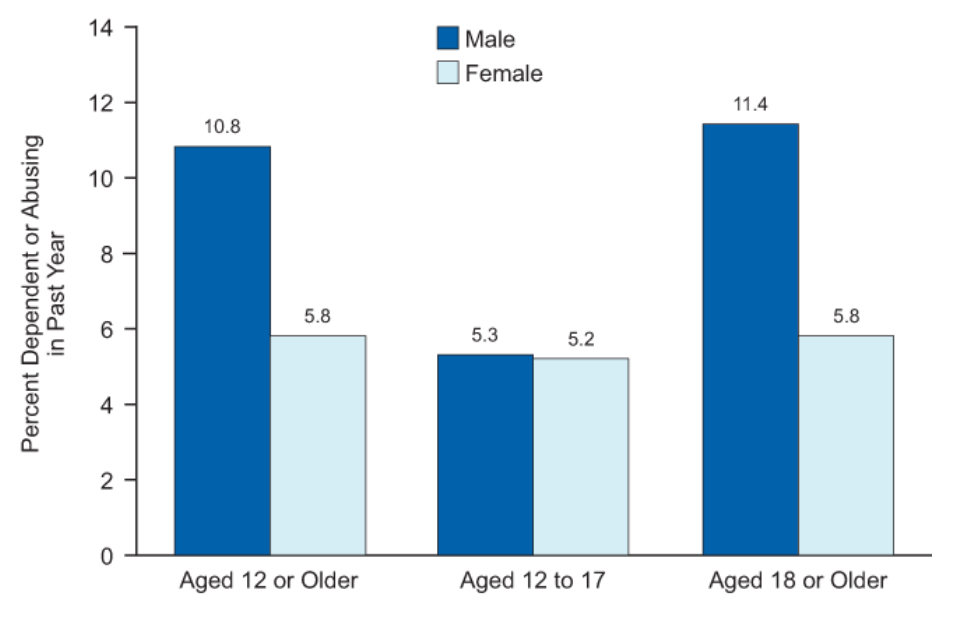
“Substance Dependence or Abuse in the Past Year, by Age and Gender: 2013” by Substance Abuse and Mental Health Services Administration (SAMHSA) is in the Public Domain
Substance Abuse Among Rural and Low-Income Men
Men are more likely to abuse illicit drugs, as men’s rates of dependency on drugs and alcohol (9.5%) are nearly double that of women (5.6%) (Substance Abuse and Mental Health Services Administration [SAMHSA], 2017). Men are at a higher risk for substance abuse; however, they are less likely to seek treatment for mental health issues, including addiction (Sagar-Ouriaghli et al., 2019). Therefore, if a man develops a substance use disorder and even acknowledges that he needs treatment, he may not receive it. This is particularly true for men in rural areas, where there are fewer prevention campaigns and treatment options/sites than in urban communities. Low-income men are also especially vulnerable to go without treatment, as many may not be able to afford it. For this reason, among others, substance abuse is an extremely prevalent issue in the population of rural and low-income men.
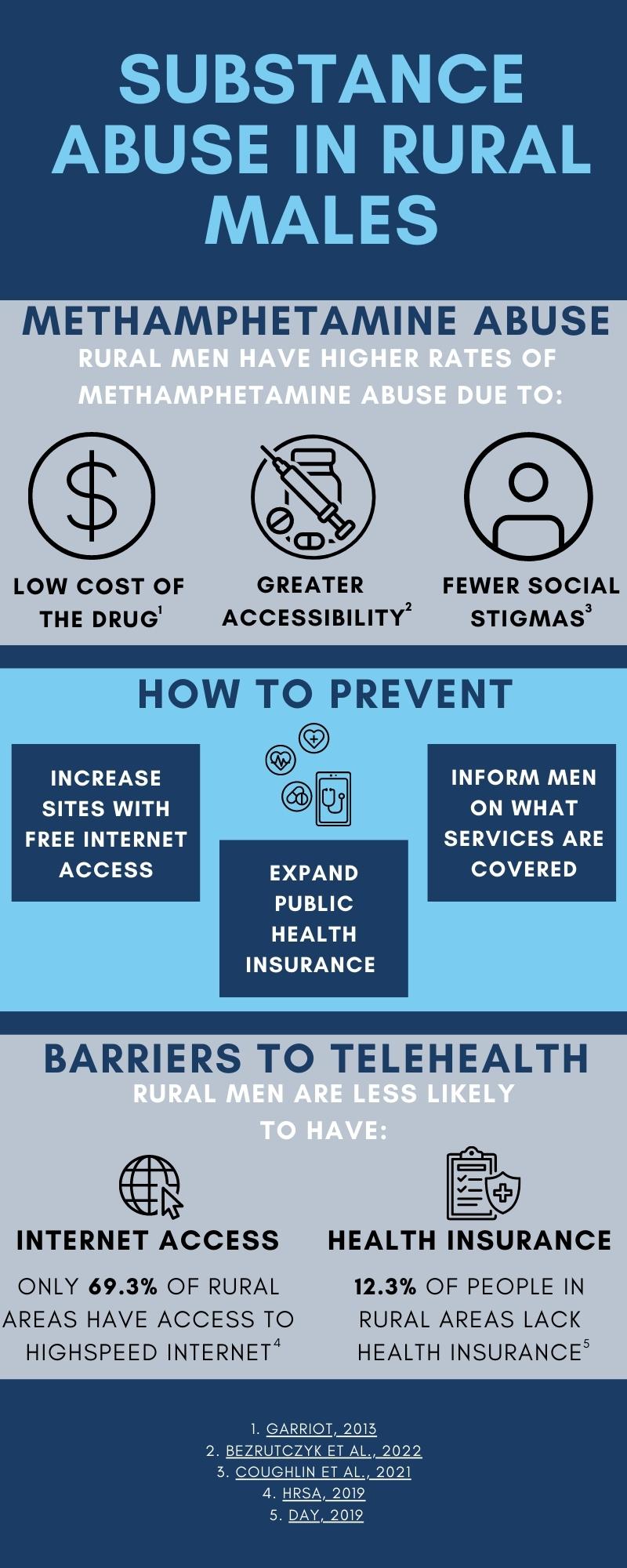
Methamphetamine Abuse
Research has shown that low-income men living in rural areas are disproportionately affected by substance abuse, namely methamphetamine. Methamphetamine, frequently referred to as “meth,” is a stimulant drug that is used to treat ADHD and help lower weight (NIDA, 2022). It is often illegally produced and has become a commonly abused drug in the United States, with 52.9% of users reporting having a methamphetamine use disorder in 2015 through 2018 (Jones et al., 2020). Rural populations have been shown to have significantly higher rates of methamphetamine use compared to those in metropolitan areas due to financial instability and inaccessibility to treatment (Jones et al., 2020). In a study that examined the sociodemographic characteristics of methamphetamine users, it was found that men who were unstably housed, low-income, and living in rural areas were more likely to use methamphetamine (Shearer et al., 2020). In addition, a study analyzing methamphetamine use among American Indians and Alaska Natives found that users were clustered in low-income, rural communities; in particular, low-income, middle-aged men had the highest rates of abuse (Coughlin et al., 2021). These higher rates of abuse could be due to an increased number of “meth labs” in rural areas, as well as the relatively low cost of methamphetamine compared to other stimulants (Bezrutczyk et al., 2022; Garriott, 2013). Having greater accessibility to methamphetamine at a low cost and less access to treatment options contribute to the increased prevalence of methamphetamine abuse in rural, low-income populations.
Opioid Abuse
Opioids are another commonly abused drug among rural and low-income men in the United States. Opioids are a highly addictive class of pain relief medications and include drugs such as heroin, fentanyl, and morphine (John Hopkins, 2022). Rural, non-metropolitan communities have higher rates of opioid abuse (3.5%) than large metropolitan areas (3.2%) (SAMHSA, 2022). In addition, opioid users are more likely to be male (Ghandour et al., 2008). According to Keyes et al. (2014), the increased rates of opioid misuse in rural populations are due to the increased availability of opioids, economic stress, and small social networks where the drug can be spread. A study on rural opioid users found that low-income, uninsured, and lowly educated individuals were more at risk of suffering adverse health outcomes due to abuse (Lenardson et al., 2016). Furthermore, rural men who abuse opioids are more likely to use them in conjunction with other drugs, increasing the risk of having adverse health outcomes (Sung et al., 2005). Research shows that users who use both methamphetamine and opioids have higher rates of chronic conditions than those who just used opioids (Shearer et al., 2020). This emphasizes the lack of substance abuse treatment resources in low-income and rural areas. If there were more accessible treatment options, the prevalence of chronic health conditions may be lowered in this population.
Substance Abuse Among Adolescent Boys
Substance abuse is not only prevalent among men, but also adolescent boys living in rural areas. A study in rural Mississippi found that boys, in grades six through eight, living in rural, low-income communities had increased rates of drug use; their rates of drug use in this community were found to be higher (Odds Ratio = 1.15-1.94) than the U.S. national averages (McDermott et al., 2013). Rural adolescents were also more likely to have past-year prescription opioid abuse (6.8%) than those in large metropolitan areas (5.3%) (Rigg & Monnat, 2015). Lower perceived risk of the drug and higher involvement in criminal activity than urban populations leads to this difference in opioid abuse (Rigg & Monnat, 2015). The lack of opioid abuse treatment options in rural areas may also play a role in the higher rates (Lenardson & Gale, 2008). Economic instability was found to lead to higher rates of substance abuse in young men as well. This association was due to the young men’s low expectations for the future, which is a factor that can increase stress, causing them to turn to substance use as a way to cope (Cho & Kogan, 2016).

Opioids and intravenous drugs, such as heroin or methamphetamine, are commonly abused drugs in rural populations.
“Drug Addiction Concept – Pills, Syringe, Heroin” by Marco Verch Professional Photographer is licensed under CC BY 2.0
Increasing Access to Treatment
Awareness of substance abuse in low-income and rural areas has grown rapidly in the past decade; however, substance abuse remains a prevalent health issue among this population, particularly men. Telehealth may be utilized to reduce the prevalence of substance abuse in rural areas where access can often be limited. Telehealth is the use of technology to receive primary healthcare, as opposed to going to an in-person appointment (Human Resources & Services Administration [HRSA], 2022). This technology allows healthcare providers to screen, evaluate, and treat patients online, as well as increase providers’ insights into the patients’ home conditions in rural settings (HRSA, 2020). Web-based models of interventions, treatment, and therapy have proven to be effective in treating substance use disorders (HRSA, 2020). Telehealth is particularly beneficial for men, who are often reluctant or embarrassed to disclose information regarding their mental health (National Library of Medicine, 2013).
Even with increased availability in rural areas, there are still factors that make access to online treatment difficult, including limited internet access and being uninsured. Those living in rural areas, specifically of low-income, are less likely to have internet availability to access telehealth than other populations (Swenson & Ghertner, 2021). A way to combat this would be to increase the number of community centers where internet access is more readily available. Offering free internet use at public libraries, churches, or other shared community spaces could effectively provide internet access to a larger portion of rural males. Another potential factor decreasing access to treatment is the lack of insurance in non-metropolitan areas. Those in rural populations are less likely to have health insurance coverage to receive treatment, emphasizing the need for more affordable coverage (Day, 2019). Policies that aim to increase the coverage of public programs, such as Medicaid, could dramatically increase the amount of treatment received by this population. It is essential to inform men about what is covered by their health insurance, as many are unaware that some services, such as treatment of substance use disorders, are covered (McKay et al., 2016). Using these methods, men who struggle with substance abuse in rural, low-income communities would then be able to utilize telehealth to get the care they need.
Key Takeaways
- Rural and low-income men are disproportionately affected by substance abuse.
- There is a lack of substance abuse treatment options in rural and remote areas.
- Telehealth services can effectively increase access to substance abuse treatments.
Chapter Review Questions
1. Rural and low-income men may recognize they need care, but may not receive it for the following reasons EXCEPT:
-
- A. Lack of treatment Options
- B. Inability to Pay
- C. Insurance won’t pay for it
- D. Stigmas surrounding receiving care
2. Adolescents in rural areas have shown to abuse prescription opioids at higher rates than urban populations. This discrepancy is due to:
-
- A. Lower perceived risk
- B. Coping mechanisms
- C. Involvement in criminal behaviors
- D. All of the above
3. Which of the following is the best definition of substance abuse?
-
- A. The excessive use of drugs that leads to negative health outcomes of the user
- B. Taking a non-prescribed drug once
- C. Using a prescribed drug as intended
- D. Using a drug on multiple occasions
4. Methamphetamine abuse may be higher in rural populations because of:
-
- A. More treatment options in these areas
- B. The high cost of the drug
- C. Increased availability of the drug
- D. More prevention programs in these areas
References
Bezrutczyk, D., Parisi, T., & Bhatt, A. (2022). How Much Do Drugs Cost: The Steep Price of Addiction. Addiction Center. https://www.addictioncenter.com/drugs/how-much-do-drugs-cost/
Cho, J., & Kogan, S. M. (2016). Risk and Protective Processes Predicting Rural African American Young Men’s Substance Abuse. American Journal of Community Psychology, 58(3-4), 422–433. https://doi.org/10.1002/ajcp.12104
Coughlin, L. N., Lin, L. A., Jannausch, M., Ilgen, M. A., & Bonar, E. E. (2021). Methamphetamine use among American Indians and Alaska Natives in the United States. Drug and Alcohol Dependence, 227, 108921. https://doi.org/10.1016/j.drugalcdep.2021.108921
Day, J. C. (2019). Rates of Uninsured Fall in Rural Counties, Remain Higher than Urban counties. United States Census Bureau. Retrieved from https://www.census.gov/library/stories/2019/04/health-insurance-rural-america.html
Gale, J. A., Lenardson, J. D., Lambert, D., & Hartley, D. (2012). (working paper). Adolescent Alcohol Use: Do Risk and Protective Factors Explain Rural-Urban Differences? Maine Rural Health Research Center. Retrieved from http://muskie.usm.maine.edu/Publications/WP48_Adolescent-Alcohol-Use-Rural-Urban.pdf.
Garriott, W. (2013). Methamphetamine in Rural America: Notes on Its Emergence. Anthropology Now, 5(1), 27–35. https://doi.org/10.5816/anthropologynow.5.1.0027
Ghandour, L. A., Martins, S. S., & Chilcoat, H. D. (2008). Understanding the patterns and distribution of opioid analgesic dependence symptoms using a latent empirical approach. International Journal of Methods in Psychiatric Research, 17(2), 89–103. https://doi.org/10.1002/mpr.232
Health Resources and Services Administration of the U.S. Department of Health and Human Services. (2019). Barriers to Telehealth in Rural Areas. Rural Health Information Hub. Retrieved from https://www.ruralhealthinfo.org/toolkits/telehealth/1/barriers
Health Resources & Services Administration of the U.S. Department of Health and Human Services. (2020). Telehealth Models. Rural Health Information Hub. Retrieved from https://www.ruralhealthinfo.org/toolkits/substance-abuse/2/treatment/care-delivery/telehealth
Health Resources and Services Administration of the U.S. Department of Health and Human Services. (2020). Substance Use and Misuse in Rural Areas. Rural Health Information Hub. Retrieved from https://www.ruralhealthinfo.org/topics/substance-use
Health Resources & Services Administration. (2022). What is Telehealth? Telehealth.HHS.gov. Retrieved from https://telehealth.hhs.gov/patients/understanding-telehealth/
Ignaszewski M. J. (2021). The Epidemiology of Drug Abuse. Journal of Clinical Pharmacology, 61 Suppl 2, S10–S17. https://doi.org/10.1002/jcph.1937
John Hopkins Medicine. (2019). Substance Abuse / Chemical Dependency. Johns Hopkins Medicine. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/substance-abuse-chemical-dependency#:~:text=Substance%20abuse%20and%20dependence%20are,be%20determined%20in%20all%20cases.
John Hopkins Medicine. (2022). Opioids. Johns Hopkins Medicine. Retrieved from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/opioids
Jones, C. M., Compton, W. M., & Mustaquim, D. (2020). Patterns and characteristics of methamphetamine use among adults — United States, 2015–2018. Morbidity and Mortality Weekly Report, 69(12), 317–323. https://doi.org/10.15585/mmwr.mm6912a1
Keyes, K. M., Cerdá, M., Brady, J. E., Havens, J. R., & Galea, S. (2014). Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health, 104(2), e52–e59. https://doi.org/10.2105/AJPH.2013.301709
Lenardson, J., & Gale, J. A. (2008). Distribution of Substance Abuse Treatment Facilities Across the Rural – Urban Continuum. Muskie School of Public Service. Retrieved from https://muskie.usm.maine.edu/Publications/rural/pb35bSubstAbuseTreatmentFacilities.pdf
Lenardson, J., Gale, J., & Ziller, E. (2016). Rural Opioid Abuse: Prevalence and User Characteristics. Rural Health Research Gateway. Retrieved from https://www.ruralhealthresearch.org/publications/1002
Mayo Foundation for Medical Education and Research. (n.d.). Drug addiction (substance use disorder). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/drug-addiction/symptoms-causes/syc-20365112
McDermott, M. J., Drescher, C. F., Smitherman, T. A., Tull, M. T., Heiden, L., Damon, J. D., Hight, T. L., & Young, J. (2013). Prevalence and sociodemographic correlates of lifetime substance use among a rural and diverse sample of adolescents. Substance Abuse, 34(4), 371–380. https://doi-org.libproxy.clemson.edu/10.1080/08897077.2013.776000
National Library of Medicine. (2013). Addressing the Specific Behavioral Health Needs of Men. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books
Newkirk, V., & Damico, A. (2014). The Affordable Care Act and Insurance Coverage in Rural Areas. KFF. Retrieved from https://www.kff.org/uninsured/issue-brief/the-affordable-care-act-and-insurance-coverage-in-rural-areas/
NIDA. (2019). Treatment Approaches for Drug Addiction DrugFacts. National Institute on Drug Abuse. Retrieved from https://nida.nih.gov/publications/drugfacts/treatment-approaches-drug-addiction
NIDA. (2020). Prevention Principles. National Institute on Drug Abuse. Retrieved from https://nida.nih.gov/publications/preventing-drug-use-among-children-adolescents/prevention-principles
NIDA. (2022). Addiction and Health. National Institute on Drug Abuse. Retrieved from https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/addiction-health
NIDA. (2022) What is Methamphetamine?. National Institute on Drug Abuse. Retrieved from https://nida.nih.gov/publications/research-reports/methamphetamine/what-methamphetamine
Office of the Assistant Secretary for Planning and Evaluation , McKay, T., Feinberg, R., Grove, L., Bir, A., & Cohen, J., Linking Low-Income Men to Medicaid and the Health Insurance Marketplace 6–7 (2016). Research Triangle Park, NC; RTI International. Retrieved from https://aspe.hhs.gov/sites/default/files/private/pdf/198726/justicebrief.pdf
Office of the Assistant Secretary for Planning & Evaluation, Swenson, K., & Ghertner, R., People in Low-Income Households Have Less Access to Internet Services – 2019 Update (2021). Retrieved from https://aspe.hhs.gov/sites/default/files/private/pdf/263601/internet-access-among-low-income-2019.pdf
Parker, R.d., Lessard, L., Abram, M.d., & Meyer, J. (2022). Twenty Years of Addiction and Mental Illness in Alaska: Using the National Survey on Drug Use and Health to Understand Addiction in a Low Population and Rural State. Journal of Community Health, 47(4), 680–686. https://doi.org/10.1007/s10900-022-01098-0
Rigg, K. K., & Monnat, S. M. (2015). Urban vs. rural differences in prescription opioid misuse among adults in the United States: informing region specific drug policies and interventions. The International Journal on Drug Policy, 26(5), 484–491. https://doi.org/10.1016/j.drugpo.2014.10.001
Sagar-Ouriaghli, I., Godfrey, E., Bridge, L., Meade, L., & Brown, J. (2019). Improving Mental Health Service Utilization Among Men: A Systematic Review and Synthesis of Behavior Change Techniques Within Interventions Targeting Help-Seeking. American Journal of Men’s Health, 13(3), 1557988319857009. https://doi.org/10.1177/1557988319857009
Shearer, R. D., Howell, B. A., Bart, G., & Winkelman, T. (2020). Substance use patterns and health profiles among US adults who use opioids, methamphetamine, or both, 2015-2018. Drug and Alcohol Dependence, 214, 108162. https://doi.org/10.1016/j.drugalcdep.2020.108162
Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality. (2017). 2016 National Survey of Drug Use and Health (NSDUH) releases. SAMHSA.gov. https://www.samhsa.gov/data/release/2016-national-survey-drug-use-and-health-nsduh-releases
Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/
Substance Abuse and Mental Health Services Administration. (2021). Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders. SAMHSA. https://www.samhsa.gov/resource/ebp/telehealth-treatment-serious-mental-illness-substance-use-disorders
Substance Abuse and Mental Health Services Administration. (2022). 2020 NSDUH Detailed Tables. SAMHSA. https://www.samhsa.gov/data/report/2020-nsduh-detailed-tables
Sung, H.-E., Richter, L., Vaughan, R., Johnson, P. B., & Thom, B. (2005). Nonmedical Use of Prescription Opioids Among Teenagers in the United States: Trends and Correlates. Journal of Adolescent Health, 37(1), 44–51. https://doi.org/10.1016/j.jadohealth.2005.02.013
United States Department of Health and Human Services . (2021). Tele-treatment for Substance Use Disorders. Telehealth.HHS.gov. https://telehealth.hhs.gov/providers/telehealth-for-behavioral-health/tele-treatment-for-substance-use-disorders/

