David Cote
Introduction

Testicular torsion occurs when the testicles rotate and the spermatic cord twists. The spermatic cord brings blood flow to the scrotum; therefore, the twisting will reduce the amount of blood getting to the scrotum, which will cause severe pain and swelling. Testicular torsion requires immediate surgical attention, and if blood flow is completely stopped, then the testicle may have to be surgically removed. It is extremely painful and permanent damage is almost certain if not treated quickly. For males younger than 18 years old, the estimated yearly frequency of testicular torsion is about 4 per 100,000 (Zhao et al., 2011). There is still no real cause for testicular torsion, although it has been found mainly in men who have an inherited trait that allows the testicle to rotate freely inside the scrotum (Mayo Foundation for Medical Education and Research, 2020). Moreover, injury to the testicles due to sports, exercise, or an accident can be associated with the onset of testicular torsion (Mayo Foundation for Medical Education and Research, 2020).
Testing
People need to seek immediate medical attention if they experience the following symptoms: severe pain or swelling in the scrotum, abdominal pain, nausea, or vomiting. One possible way for a doctor to assess if a patient has testicular torsion is through the TWIST (Testicular Workup for Ischemia and Suspected Torsion) score. The Canadian Medical Association Journal writes, “Scoring is as follows: testicular swelling (2 points), hard testis (2 points), absent cremasteric reflex (1 point), nausea and vomiting (1 point), and high-riding testis (1 point)” (Keays & Rosenberg, 2019). Scoring of 0 means that there is no indication of testicular torsion, whereas a score of 6 or 7 is highly predictive of testicular torsion. Another testing method used is an ultrasound, which can detect structural issues and the amount of blood flow to the testes (El-Feky et al., 2021). Ultrasound results can show twisting of the spermatic cord, altered blood flow, increase in the size of the testis, and thickening of the scrotal skin with hyperemia (El-Feky et al., 2021).
More Common in Boys Than Men
Testicular torsion is seen most commonly in both young adults and babies that are four weeks old or younger. Testicular torsion in young adults is more common due to the bell clapper deformity. Bell clapper deformity is something that affects the spermatic cord in such a way to allow the testis to move more freely. This occurs in 5%-16% of males and increases the risk of the spermatic cord getting twisted (El-Feky et al., 2021). One study performed by the Journal of Urology showed the distribution of testicular torsion to peak in the first year of life and early adolescence (Zhao et al., 2011). The study also revealed that orchiectomies were performed on about 42% of boys undergoing surgery for torsion. Orchiectomy rates were highest in kids younger than 10 years old, and there was an increased frequency of orchiectomy among cases in the Black race (Zhao et al., 2011). Since this is an irregular condition, there is no difference in saving the testicle among different races (Ramachandra et al., 2015).
Repair and Future Effects
Surgery is the only practical option for a patient with twisted testicles in order to save the testicles. In order to perform the surgery, the surgeon will cut the scrotum to gain access to the twisted spermatic cord. The cord will be untwisted, and then the surgeon will stitch the testicle to the scrotum. The surgeon will do this to both testicles to prevent future problems by not allowing the testicles to move freely inside the sac. If one testicle has to be removed, the other testicle should be able to provide enough hormones for male growth, sex life, and fertility (Shah, 2019). When surgical correction is performed within 6 hours of the start of testicular torsion, there is 90%-100% survival rate of the testicle. However, when surgery is performed within 12-24 hours from the start of testicular torsion, there is only 10% survival rate of the testicle (Keays & Rosenberg, 2019). Although more research needs to be done, there is some notice of lower sperm quality after testicular torsion. Moreover, animal studies have demonstrated testicular torsion’s negative impact on the testis opposite of the twisted testis. The impact is due to blood supply returning rapidly after a period of absence of oxygen (Jacobsen et al., 2020).
Prevention
Although there is no clear prevention for testicular torsion besides surgery, awareness of it can help to avoid permanent damage. A study done by Children’s Health (n.d.) found that males under 18 years old waited up to 20 hours before going to the emergency room. Although it may be uncomfortable to talk to a parent about genital problems, boys need to speak up to prevent further problems in the future. Also, it could never hurt to wear proper protection during sports in order to prevent direct contact with the testicles. However, the only true way to stop future testicular torsion is by stitching the testicle to the scrotum through testicular torsion repair surgery.
Summary of Testicular Torsion

Chapter Review Questions
1. What is the only actual way to prevent testicular torsion from occurring?
A. There is no way to prevent testicular torsion
B. Stitching the testicle to the scrotum through surgery
C. Exercising on a daily basis
D. Massaging the testicle to increase blood flow
2. What is the survival rate of a testicle when surgery is performed within 12-24 hours from the onset of testicular torsion?
A. 90%
B. 50%
C. 10%
D. 42%
3. Which of the following symptoms is concurrent with testicular torsion?
A. Difficulty urinating
B. High fever
C. Intense itching of the groin
D. Abdominal pain
References
El-Feky, M., Gaillard, F., & Hacking, C. (2021, April 13). Testicular torsion. Radiopaedia. https://radiopaedia.org/articles/testicular-torsion
Jacobsen, F. M., Rudlang, T. M., Fode, M., Østergren, P.,B., Sønksen, J., Ohl, D. A., Jensen, C. F. S., & Collaborative, C. (2020). The impact of testicular torsion on testicular function. The World Journal of Men’s Health, 38(3), 298-307. 10.5534/wjmh.190037
Keays, M., & Rosenberg, H. (2019). Testicular torsion. CMAJ: Canadian Medical Association Journal, 191(28), E792. 10.1503/cmaj.190158
Mayo Foundation for Medical Education and Research. (2020, April 4). Testicular torsion. Mayo clinic. https://www.mayoclinic.org/diseases-conditions/testicular-torsion/symptoms-causes/syc-20378270
Ramachandra, P., Palazzi, K. L., Holmes, N. M., & Marietti, S. (2015). Factors influencing rate of testicular salvage in acute testicular torsion at a tertiary pediatric center. The Western Journal of Emergency Medicine, 16(1), 190-194. 10.5811/westjem.2014.11.22495
Shah, S. M. (2019, July 31). Testicular torsion repair. MedlinePlus. https://medlineplus.gov/ency/article/002994.htm
Children’s Health. (n.d.). Testicular torsion: Signs, causes and what to do. https://www.childrens.com/health-wellness/testicular-torsion-signs-causes-what-to-do.
Zhao, L. C., Lautz, T. B., Meeks, J. J., & Maizels, M. (2011). Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. The Journal of Urology, 186(5), 2009-2013. 10.1016/j.juro.2011.07.024
Introduction
The SARS-CoV-2 virus, also known as COVID-19, is a sickness that affects the respiratory tract. It was first discovered in 2019 and has spread across the entire world. Within a year, 27 million cases were reported in the United States. And of those, there were almost half a million deaths (Center for Disease Control, 2021). Research has found that men are dying from COVID-19 at a disproportionate rate when compared to women. In Italy, the death rate of men with COVID-19 was 13.3%, compared to 7.4% for women. (Pivonello et al., 2020). Because of this difference, it is important for men to know the symptoms, why they are at a greater risk, and how they can decrease the severity of COVID-19.
What Are COVID-19 Symptoms?
Some of the virus’s most common symptoms include fever, dry cough, headaches, loss of taste and/or smell, and digestive issues (Pivonello et al., 2020). Around 80% of cases will produce these mild to moderate symptoms (Giagulli et al., 2021). Some people will develop severe symptoms that lead to hospitalizations. This is much more common in older patients or those with pre-existing medical conditions (Giagulli et al., 2021). Other cases present as asymptomatic, which means that the person experiences no symptoms and therefore is unaware that they have the virus.
Why Are Men More at Risk for Severe Disease?
Men, compared to women, are at a biological disadvantage because of their immune system’s response to this type of virus. This means that men’s and women’s bodies react differently to the virus, simply because of sex differences. Many genes that are related to the immune system and someone’s response to germs are located on the X chromosome (Pivonello et al., 2020). Women have two X chromosomes, meaning if they have a mutation on one, it is possible that the other X chromosome will hide it. Since men only have one X chromosome, if they have a mutation that disrupts their immune response it cannot be hidden (Pivonello et al., 2020). Mutations on the Y chromosome, only found in men, can also suppress the immune system response (Pivonello et al., 2020).
Additionally, testosterone has a suppressive effect on the immune system. Women have small amounts of testosterone, but not nearly as much as men. Testosterone has been shown to reduce white blood cell levels which can decrease the production of immunoglobin E, which helps the body fight off bacteria, viruses, and allergens, and is therefore very important for someone to have when fighting COVID-19 (Giagulli et al., 2021).
How Can Men Prevent Becoming Infected With COVID-19?
Because of these biological disadvantages, men need to be more proactive about other health behaviors in order to decrease their risk of developing a severe case of COVID-19. Men are more likely to participate in risky behavior which can include behaviors like not wearing masks or social distancing that could expose them to the virus more often than women. Additionally, according to the CDC, more men have reported going to social gatherings during the pandemic than women (Griffith et al., 2020). Until the majority of the world is vaccinated, it is very important that everyone, but especially men, wear protective masks in order to minimize the risk of contracting and spreading the virus.
Not only does risky behavior pose a threat to men contracting the virus, but certain pre-existing conditions can also put men at risk. According to the Australasian Journal of Medicine, two separate studies performed in Italy and New York calculated the percentage of people who died from COVID-19 that had other medical conditions. In Italy, out of 355 deaths studied, only 1 person had no other existing conditions. In New York, over 13,000 people were included in the study and 89% of them had a chronic condition. These conditions included but were not limited to: hypertension, diabetes, coronary heart disease, chronic lung diseases, chronic kidney disease, and congestive heart failure (Cumming et al., 2020). Additionally, those with low vitamin D levels are predisposed to COVID-19. Those with this deficiency should take vitamin supplements to help boost their immune system function (Abdollahi et al., 2021). This means that men need to be more aware of their diet and negative health behaviors that can contribute to other diseases and therefore affect their likelihood of getting COVID-19.
The Importance of Vaccination
While there still is no cure for this deadly virus, vaccines are available to the general public, and they can help reduce the risk of a severe COVID-19 infection. Because of the contagious nature of COVID-19, it is very important for everyone to vaccinate, as long as they are able, in order to slow the spread of the virus. Some men can be resistant to vaccines because they can be costly, they can be painful, and they are uneducated about the benefits (Snyder, 2020). Vaccination rates can not only vary among males and females but also by ethnicity and race. Multiple studies found that around 20% of Mexican-American men regularly participated in getting the flu vaccine in 2015, which is a much lower percentage compared to other ethnic groups (Snyder, 2020). Because of this, it is important that healthcare and prevention strategies for COVID-19 target all groups of men and not generalize men into one category.

Chapter Review Questions
1. What is the most effective way to prevent a severe case of COVID-19?
A. Wearing a mask
B. Social distancing
C. Vaccination
D. Double-masking
2. What is an uncontrollable factor that puts men more at risk for contracting COVID-19?
A. Vitamin D levels
B. Mutations on chromosomes
C. Pre-existing conditions
D. Risky behaviors
3. How do chromosomes contribute to increased mutations on men’s genes?
A. Men only have one X chromosome, and it cannot be masked
B. Men's Y chromosome has an increased likelihood of having a mutation
C. Men have more exposure to toxins that cause mutations compared to women
D. The mutations are due to higher levels of testosterone in the body compared to women
References
Abdollahi, A., Sarvestani, H. K., Rafat, Z., Ghaderkhani, S., Mahmoudi-Aliabadi, M., Jafarzadeh, B., & Mehrtash, V. (2021). The association between the level of serum 25(OH) vitamin D, obesity, and underlying diseases with the risk of developing COVID-19 infection: A case-control study of hospitalized patients in Tehran, Iran. Journal of Medical Virology., 93(4), 2359-2364. https://doi.org/10.1002/jmv.26726
Center for Disease Control. (2021). COVID data tracker. Retrieved February 14, 2021, from https://covid.cdc.gov/covid-data-tracker/#global-counts-rates
Cumming, R., Khalatbari-Soltani, S., Blyth, F. M., Naganathan, V., & Le Couteur, D. G. (2020). Not all older men have the chronic diseases associated with severe COVID‐19. Australasian Journal on Ageing, 39(4), 381–382. https://doi.org/10.1111/ajag.12839
Giagulli, V. A., Guastamacchia, E., Magrone, T., Jirillo, E., Lisco, G., De Pergola, G., & Triggani, V. (2021). Worse progression of COVID-19 in men: Is testosterone a key factor? Andrology, 9(1), 53–64. https://doi.org/10.1111/andr.12836
Griffith, D. M., Sharma, G., Holliday, C. S., Enyia, O. K., Valliere, M., Semlow, A.R., Stewart, E. C., & Blumenthal, R. S. (2020) Men and covid-19: A biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Preventing Chronic Disease, 17. http://dx.doi.org/10.5888/pcd17.200247
Pivonello, R., Auriemma, R. S., Pivonello, C., Isidori, A. M., Corona, G., Colao, A., & Millar, R. P. (2020). Sex disparities in covid-19 severity and outcome: Are men weaker or women stronger? Neuroendocrinology. https://doi-org.libproxy.clemson.edu/10.1159/000513346
Snyder, V., Garcia, D., Pineda, R., Calderon, J., Diax, D., Morales, A., & Perez, B. (2020). Exploring why adult mexican males do not get vaccinated: Implications for COVID-19 preventive actions. Hispanic Journal of Behavioral Sciences, 42(4), 515–527. https://doi-org.libproxy.clemson.edu/10.1177/0739986320956913
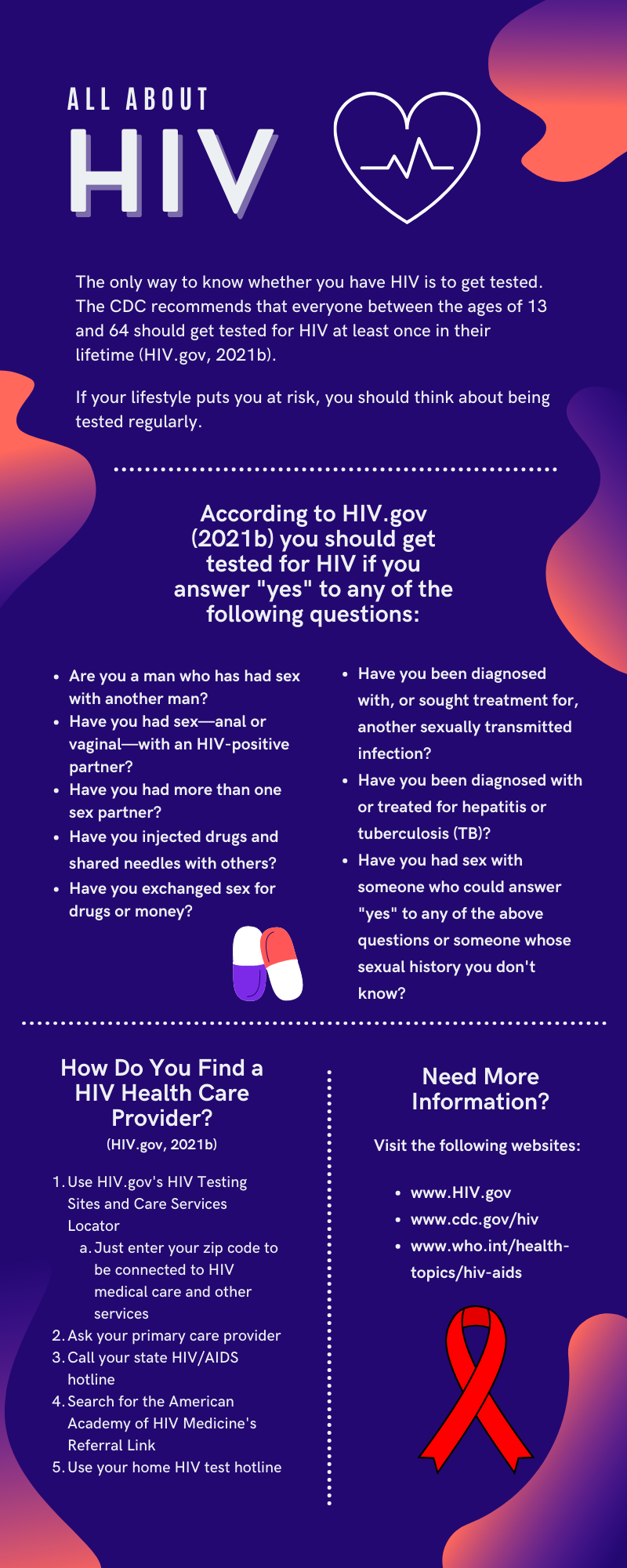
What is HIV?
According to HIV.gov (2021a), the human immunodeficiency virus, otherwise known as HIV, is a virus that attacks the body's cells that helps fight infection, making an individual more at risk for other diseases and infections. HIV spreads by having contact with certain bodily fluids such as blood, semen, or urine of an HIV-positive person. The most common forms of spreading HIV are participating in unprotected sex and sharing injection drug needles. If HIV is left untreated, it can lead to the development of AIDS, acquired immunodeficiency syndrome. Currently, there is no cure for HIV, so once someone tests positive, they will be dealing with the symptoms for life.
Symptoms of HIV
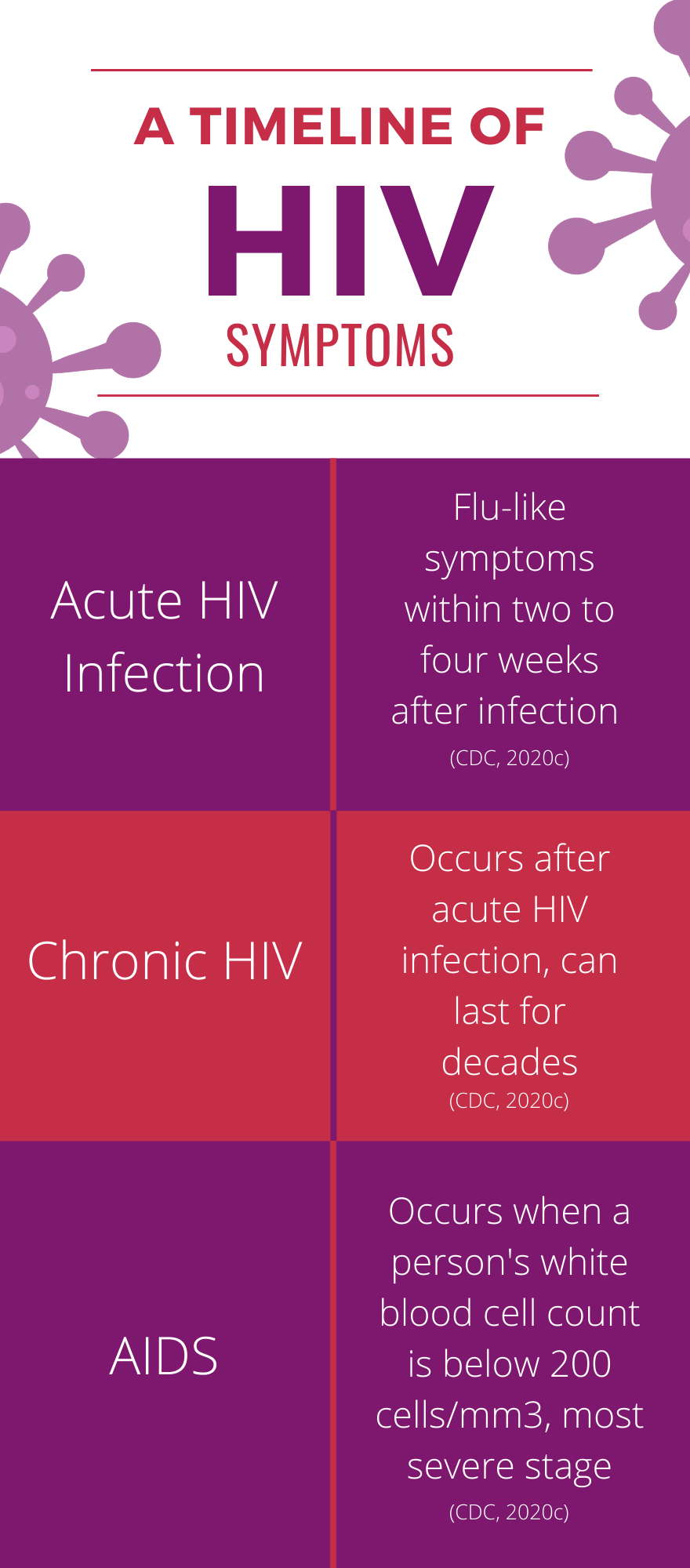
The Center for Disease Control and Prevention (CDC) (2020c) states that some individuals will have flu-like symptoms within two to four weeks after infection, otherwise known as acute HIV infection. These symptoms might last for a couple of days or several weeks. Potential symptoms include fever, chills, rash, night sweats, muscle aches, sore throat, fatigue, swollen lymph nodes, and mouth ulcers. Some individuals, however, might not feel sick during the acute stage of HIV infection. It is important to note that these symptoms alone do not necessarily mean you have HIV. Multiple other illnesses can cause these same symptoms, and getting tested for HIV is the only sure way to know.
Stages of HIV
The CDC (2020c) describes the stage symptoms in the following manner. Stage one is the acute HIV infection period of two to four weeks after first exposure. Some individuals have flu-like symptoms as listed above, but individuals may not feel sick right away or at all. Stage 2 is the chronic HIV infection period after acute infection. Symptoms can range from mild to severe, depending on how advanced the infection is, including coughing or breathing difficulties, weight loss, diarrhea, fatigue, or high fever. Stage 3 is when a person's white blood cell count is low, and they are diagnosed with AIDS, the final and most severe phase of HIV infection. People with AIDS have badly damaged immune systems and can often develop several severe illnesses at an increased rate. The survival rate without treatment is about three years; however, with the development and availability of current HIV medications, an individual’s progression into stage three is less common today than in the 1980s. In some cases, people with chronic HIV will have no symptoms, otherwise known as a latent infection, lasting up to ten years.
Who Is At Risk for HIV?
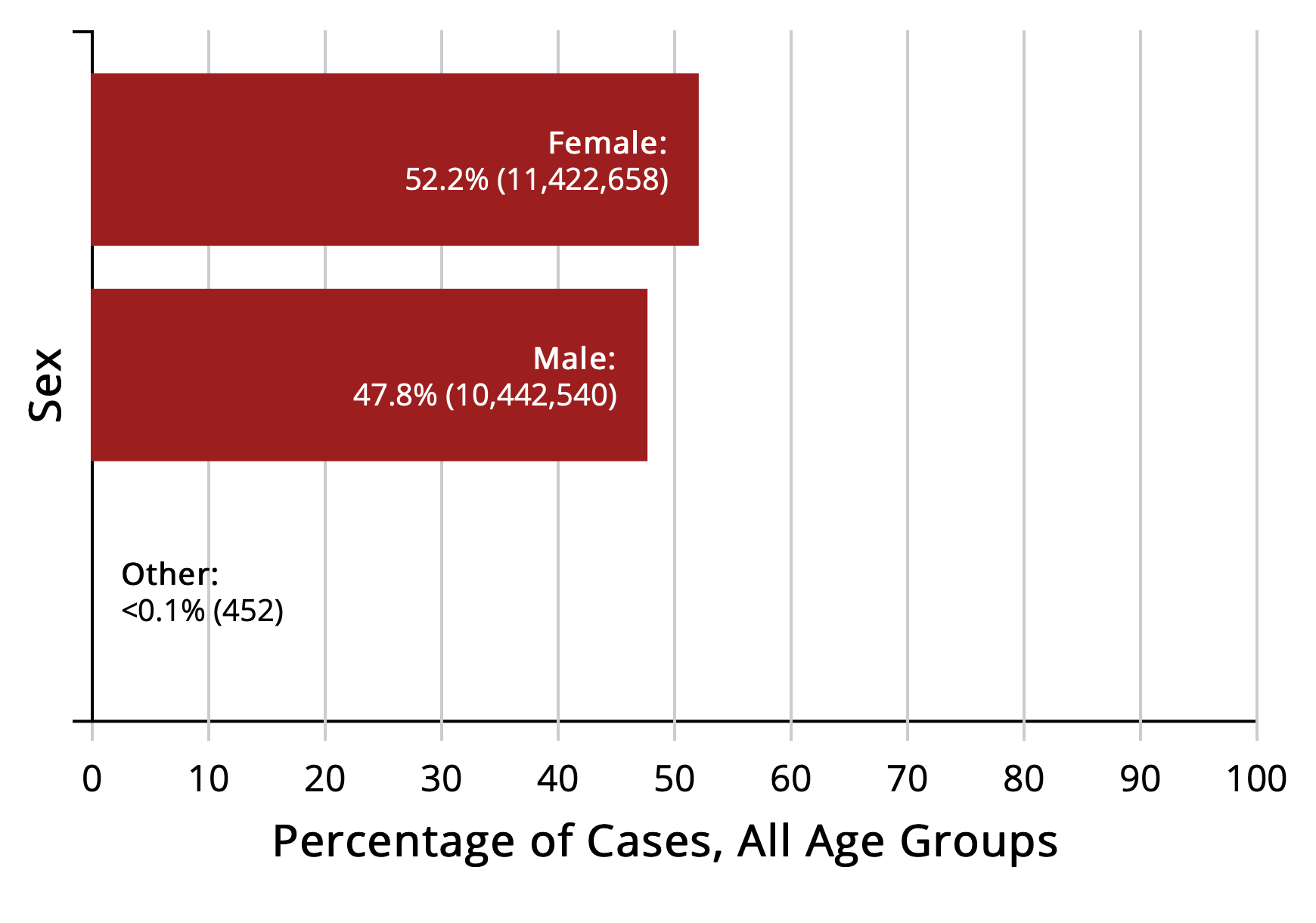
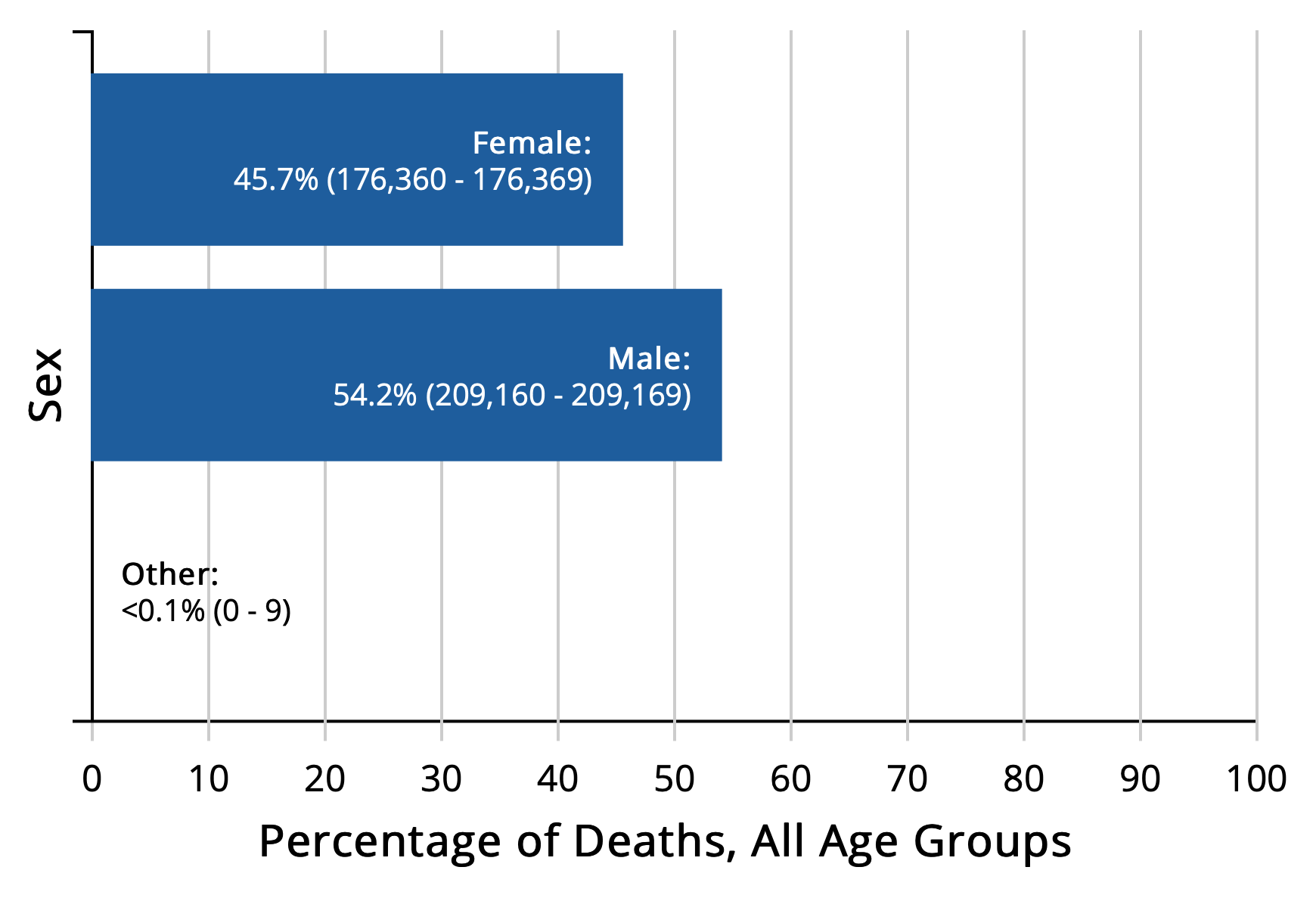
HIV can affect anyone regardless of age, gender, race, ethnicity, sexual orientation, or where they live. However, certain groups of people in the United States are more likely to get HIV than others because of certain factors, including what subpopulations they belong to and their risk behaviors. In 2018, men accounted for 81% of the 37,968 new HIV diagnoses in the United States (CDC, 2020g). Nearly one in seven men with HIV are unaware they have it (CDC, 2020g). According to CDC (2020a), gay and bisexual men accounted for 69% of new HIV diagnoses in 2018, making them the population most affected by HIV. The spread of HIV and other sexually transmitted infections among gay and bisexual men has become a syndemic. The specific health problems that have created the HIV syndemic include the number of infectious diseases regularly found among this particular population, the high rate of substance abuse problems and psychological disorders, and the significant percentage of gay and bisexual men who have experienced childhood sexual abuse and other negative events (O’Leary, 2014, p. 22).
HIV Prevention
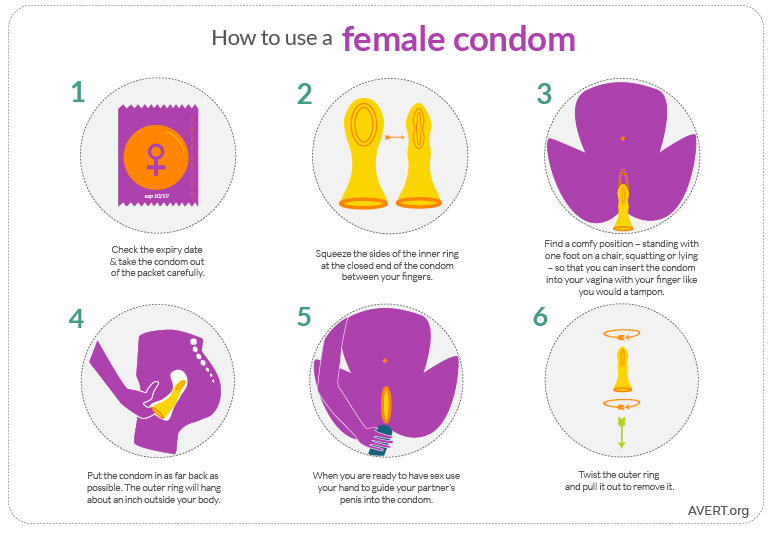
On their website, the CDC (2021) outlines the many tools that can help prevent HIV. One of the most popular ways to prevent HIV when engaging in sex is wearing a condom. Most condoms are highly effective in preventing HIV as well as other sexually transmitted infections. There are two main types of condoms: external condoms and internal condoms. An external condom, also known as a male condom or just a condom, is worn over the penis during sex. Latex condoms provide the most protection against HIV. Natural membrane, such as lambskin, condoms have small holes in them and do not block HIV and other STI’s. Individuals should not use natural membrane condoms for HIV or STI prevention. An internal condom, also known as the female condom, is used in the vagina or anus during sex. A female condom is a thin pouch made from nitrile, which is a synthetic latex product. HIV can not travel through the nitrile barrier.

Another way to prevent HIV when engaging in sex or injection drug use is by taking pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP). PrEP is medicine for individuals at risk for HIV to prevent getting HIV. When taken as prescribed by healthcare providers, PrEP is about 99% for preventing the risk of contracting HIV from sex (CDC, 2020e). Although there is not as much information about how effective PrEP is among people who inject drugs, there is enough information to conclude that PrEP reduced the risk of getting HIV by at least 74% when taken as prescribed (CDC, 2020f). PEP is a medicine taken to prevent HIV after a possible exposure. The CDC (2020d) recommends that PEP should only be used for emergencies and needs to start within 72 hours after unprotected sex or infected blood from a needle.
HIV Stigma and Discrimination
HIV stigma refers to the negative beliefs and attitudes directed at people living with HIV and AIDS. It is the bias that comes from identifying a person as part of a group that is understood to be socially unacceptable. Examples from the CDC (2020b) include:
- Thinking that only certain groups of people can get HIV.
- Making judgments about people who take action to prevent HIV transmission.
- Feeling that individuals deserve to get HIV because of their actions.
While stigma pertains to a belief or attitude, discrimination is the conduct that comes from those beliefs or attitudes. HIV discrimination is treating individuals living with HIV differently than those without HIV. Examples include a health care professional refusing to provide care to a person living with HIV, socially cutting off a community member because they are HIV positive, and referring to people as Positives or HIVers (CDC, 2020b).
HIV stigma today comes from the many negative beliefs about HIV when HIV first appeared in the early 1980s. Yet, there are still many misunderstandings today about how HIV is transmitted and what it means to live with HIV. The lack of awareness and information linked with out-of-date ideas leads individuals to fear HIV (CDC, 2020b).
HIV affects the body not only physically but also mentally. Individuals with HIV often internalize the stigma they face and begin to grow a poor self-image. These individuals may worry about their HIV status being shared because they may be judged or face prejudice. HIV internalized stigma can bring on feelings of shame, isolation, fear of sharing, and hopelessness. Stigma and discrimination can keep individuals from getting tested and treated for HIV (CDC, 2020b).
Life After an HIV Positive Diagnosis
Being HIV-positive can be an overwhelming and lonely experience. However, many organizations and resources, such as the Joint United Nations Programme on HIV/AIDS and the Kaiser Family Foundation, are available to help the more than one million HIV-positive people living in the United States today (HIV.gov, 2020). Also, remember that being HIV-positive is not the death sentence it once was. HIV can lead to AIDS, but being HIV-positive does not necessarily mean that an individual has AIDS. New treatments have allowed HIV to develop into a more stable condition. With the proper medical care and a healthy lifestyle, many HIV-positive individuals can live full lasting lives (WebMD, 2007).
Chapter Review Questions
1. If you know you have been exposed to HIV, when is the latest that you can take post-exposure prophylaxis (PEP)?
A. 24 hours after exposure
B. 72 hours after exposure
C. 48 hours after exposure
D. 1 week after exposure
2. What is one way HIV is spread?
A. Physical touch
B. Toilet seats
C. Blood
D. Insects
3. What type of condom material does not protect you from HIV?
A. Latex
B. Polyurethane
C. Natural membrane
D. All condoms protect from HIV
References
Centers for Disease Control and Prevention. (2020a, September 16). HIV and Gay and Bisexual Men. https://www.cdc.gov/hiv/group/msm/index.html
Centers for Disease Control and Prevention. (2020b, October 22). HIV Stigma. https://www.cdc.gov/hiv/basics/hiv-stigma/index.html
Centers for Disease Control and Prevention. (2020c, November 3). About HIV/AIDS. https://www.cdc.gov/hiv/basics/whatishiv.html
Centers for Disease Control and Prevention. (2020d, November 3). About PEP. https://www.cdc.gov/hiv/basics/pep/about-pep.html
Centers for Disease Control and Prevention. (2020e, November 3). PrEP. https://www.cdc.gov/hiv/basics/prep.html
Centers for Disease Control and Prevention. (2020f, November 3). PrEP Effectiveness. https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html
Centers for Disease Control and Prevention. (2020g, November 5). HIV and Men. https://www.cdc.gov/hiv/group/gender/men/index.html
Centers for Disease Control and Prevention. (2021, February 11). Condoms. https://www.cdc.gov/hiv/basics/hiv-prevention/condoms.html
HIV.gov. (2020, November 5). Global HIV/AIDS organizations. https://www.hiv.gov/federal-response/pepfar-global-aids/global-hiv-aids-organizations
HIV.gov. (2021a, January 26). What are HIV and AIDS? https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/what-are-hiv-and-aids
HIV.gov. (2021b, January 26). Who should get tested? https://www.hiv.gov/hiv-basics/hiv-testing/learn-about-hiv-testing/who-should-get-tested
O’Leary, D. (2014). The syndemic of AIDS and STDS among MSM. The Linacre Quarterly, 81(1), 12–37. https://doi.org/10.1179/2050854913y.0000000015
WebMD. (2007, February 1). What to Do After Being Diagnosed As HIV-Positive. https://www.webmd.com/hiv-aids/hiv-positive-what-now
an asymptomatic abnormal state that precedes the development of clinically evident diabetes
a crystalline sugar C6H12O6. Specifically: the sweet colorless soluble dextrorotatory form that occurs widely in nature and is the usual form in which carbohydrate is assimilated by animals
chronic inability to achieve or maintain an erection satisfactory for sexual intercourse

