11 High Blood Pressure
Perry Fleming
Introduction
High blood pressure, or hypertension (HTN), is a major problem in the U.S. Currently, 108 million U.S. adults (50%) have been diagnosed with it, and only about 25% have it under control (Centers for Disease Control and Prevention [CDC], 2020). If not successfully managed, HTN is very dangerous, leading to heart disease or stroke (Kjeldsen, 2018). Indeed, in 2019 HTN contributed to nearly 500,000 deaths in the U.S. (CDC, 2020). While the risk of developing this disease increases with age, college-aged men are also affected (Kjeldsen 2018). A recent study showed that 27% of men in their twenties were hypertensive (Everett & Zajacova, 2015). Therefore, it is crucial for college-aged men to be informed and take preventative actions early in life.
What is High Blood Pressure?
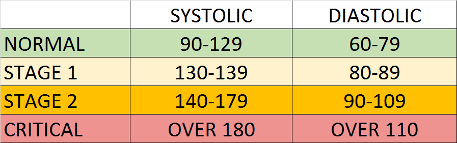
Blood pressure is the pressure that blood puts on the blood vessel walls. If blood pressure is constantly high, it can cause damage to these vessels and promote cardiovascular problems (Stevens et al., 2016). There are four blood pressure categories: normal, stage 1, stage 2, and critical (see figure). Blood pressure is measured by the systolic pressure (first or top number) and diastolic pressure (second or bottom number). Specifically, HTN is defined as blood pressure higher than 130/80 mm Hg. Typically, an HTN diagnosis is made by health professionals after several measurements over a period of time. As blood pressure increases, the risk of a sudden heart attack or stroke increases dramatically. Therefore, it is important to keep blood pressure under control.
There are two main categories of HTN: essential (also known as primary) and secondary. The majority of patients (95-98%) have essential HTN. For this type, there is no single identifiable cause of the disease, but rather multiple interrelated causes (Beevers et al., 2001). It is most likely that the majority of college-aged males with HTN would fall in the essential HTN group. Secondary HTN, which only 2-5% of patients have, is classified as HTN due to an underlying kidney or adrenal gland disease.
HTN prevalence varies between males and females depending on age. Generally, more men have HTN than women, but there is not always a major difference. Recent data from 2015-2018 showed that in the U.S., more men have HTN up to age 64, but more women have HTN after age 64 (Virani et al., 2020). There are several reasons for the observed age and gender differences in HTN prevalence. One reason is that women are more protected because of the effects of estrogens before menopause. However, other reasons could be due to differences in salt sensitivity between men and women or that men have an increased likelihood of developing problems with their hearts (Doumas et al., 2013).
High Blood Pressure Awareness and Treatment

High blood pressure is often known as the “silent killer” because it is not associated with major symptoms. Many people, including college-aged men, do not even realize they have HTN. A 2015 study found that only 25% of men in their twenties were aware of their hypertensive status (Everett & Zajacova, 2015). Therefore, it is important to get regular blood pressure checks to screen for HTN. It is recommended that adults 18 years or older with normal blood pressure and no risk factors be rescreened every 3-5 years. However, adults ≥40 years old or persons at an increased risk for HTN should be rescreened annually (United States Preventative Services Task Force, 2016). Several studies have shown that treatment can effectively reduce HTN (Hermida et al., 2013). Unfortunately, less than 50% of people (mostly ≤40 years old) continue to take their medications after one year (Burnier & Egan, 2019). These statistics are mainly due to the perceived side effects of the medications. However, it is best to discuss other treatment methods with a physician rather than having no treatment at all.
Preventing High Blood Pressure
There are many steps men can take to reduce the risk of developing HTN. First, it is essential to eat healthy foods and get plenty of exercise. It has been found that proper diet and exercise (both aerobic and strength training) are effective at lowering high blood pressure (Jurik & Stastny, 2019). Additionally, there is some evidence that high sodium intake raises blood pressure (He et al., 2012). It is estimated that the average American eats close to 1,000 mg over the recommended sodium intake levels (Strazzullo & Leclercq, 2014). Therefore, it is best to eat fresh produce and minimize large quantities of high-sodium packaged foods.
Conclusion
Overall, it is crucial for men to understand this disease at an early age. Early preventative measures could save men $190,000, which is the average lifetime cost of HTN treatment (Doumas et al., 2013). While HTN is widespread, new technologies are improving HTN treatment. Smartphones and wearable Bluetooth blood pressure measuring devices are becoming increasingly common in HTN management. It is expected that these technologies will continue to develop and can support people with active lifestyles (Kitt et al., 2019). Although treatment is improving, college-aged men should continue to treat this disease seriously, maintain a healthy lifestyle, and educate peers on the dangers of this silent killer.
Chapter Review Questions
1. Which of the following blood pressure measurements are in the critical range?
A. 95/65 mm Hg
B. 120/80 mm Hg
C. 150/90 mm Hg
D. 190/115 mm Hg
2. Which condition is most associated with hypertension?
A. Kidney stones
B. Stroke
C. Lung cancer
D. Sickle cell anemia
3. Why is hypertension known as the silent killer?
A. Patients do not talk about the disease
B. It does not cause major symptoms
C. Doctors cannot hear blood flow
D. It is an infectious disease
References
Beevers, G., Lip, G. Y. H., & O’Brien, E. (2001). The pathophysiology of hypertension. BMJ: British Medical Journal, 322(7291), 912-916. 10.1136/bmj.322.7291.912
Burnier, M., & Egan, B. M. (2019). Adherence in hypertension: A review of prevalence, risk factors, impact, and management. Circulation Research, 124(7), 1124–1140. 10.1161/CIRCRESAHA.118.313220
Centers for Disease Control and Prevention. (2020, September 8). Facts about hypertension. https://www.cdc.gov/bloodpressure/facts.htm
Doumas, M., Papademetriou, V., Faselis, C., & Kokkinos, P. (2013). Gender differences in hypertension: myths and reality. Current Hypertension Reports, 15(4), 321–330. 10.1007/s11906-013-0359-y
Everett, B., & Zajacova, A. (2015). Gender differences in hypertension and hypertension awareness among young adults. Biodemography and Social Biology, 61(1), 1-17. 10.1080/19485565.2014.929488
He, F. J., Campbell, N. R., & MacGregor, G. A. (2012). Reducing salt intake to prevent hypertension and cardiovascular disease. Revista Panamericana de Salud Pública, 32(4), 293–300. 10.1590/s1020-49892012001000008
Hermida, R. C., Ayala, D. E., Mojon, A., & Fernández, J. R. (2013). Cardiovascular risk of essential hypertension: Influence of class, number, and treatment-time regimen of hypertension medications. Chronobiology International, 30(1–2), 315–327. 10.3109/07420528.2012.701534
Jurik, R., & Stastny, P. (2019). Role of nutrition and exercise programs in reducing blood pressure: A systematic review. Journal of Clinical Medicine, 8(9), 1393. 10.3390/jcm8091393
Kitt, J., Fox, R., Tucker, K. L., & McManus, R. J. (2019). New approaches in hypertension management: A review of current and developing technologies and their potential impact on hypertension care. Current Hypertension Reports, 21(6), 44. 10.1007/s11906-019-0949-4
Kjeldsen, S. E. (2018). Hypertension and cardiovascular risk: General aspects. Pharmacological Research, 129, 95–99. 10.1016/j.phrs.2017.11.003
Strazzullo, P., & Leclercq, C. (2014). Sodium. Advances in Nutrition, 5(2), 188–190. https://doi.org/10.3945/an.113.005215
Stevens, S. L., Wood, S., Koshiaris, C., Law, K., Glasziou, P., Stevens, R. J., & McManus, R. J. (2016). Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. British Medical Journal, 354., i4098. 10.1136/bmj.i4098
United States Preventative Services Task Force. (2016). Screening for high blood pressure in adults: recommendation statement. American Family Physician, 93(4), 300-302. https://www.aafp.org/afp/2016/0215/p300.html
Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., Chamberlain, A. M., Chang, A. R., Cheng, S., & Delling, F. N. (2020). Heart disease and stroke statistics—2020 update: A report from the American Heart Association. Circulation, 141(9), e139–e596. 10.1161/cir.0000000000000757
Whelton, P., Carey, R., Aronow, W., Casey, D., Collins, K., Dennison, H., DePalma, S., Gidding, S., Jamerson, K., Jones, D., MacLaughlin, E., Muntner, P., Ovbiagele, B., Smith, S., Spencer, C., Stafford, R., Taler, S., Thomas, R., Williams, K., … Wright, J. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension, 71(6), e13–e115. 10.1161/HYP.0000000000000066
An abnormal condition of the heart and/or blood circulation.
Sudden impairment or loss of consciousness, sensation, and voluntary motion that is caused by rupture or obstruction of a blood vessel supplying the brain.
The pressure of the arteries when the heart contracts.
The pressure of the arteries when the heart refills with blood.
either of a pair of complex endocrine organs near the anterior medial border of the kidney consisting of a mesodermal cortex that produces glucocorticoid, mineralcorticoid, and androgenic hormones and an ectodermal medulla that produces epinephrine and norepinephrine.
The proportion of a population who have a specific characteristic in a given time period.
A category of sex hormone responsible for the development and regulation of the female reproductive system and secondary sex characteristics.
the natural cessation of menstruation that usually occurs between the ages of 45 and 55.
The acute blood pressure change in mean blood pressure corresponding to a decrease or increase of sodium intake.
Exercises such as jogging, rowing, swimming, or cycling, that stimulate and strengthen the heart and lungs, thereby improving the body's use of oxygen.

