15 Prostate Cancer
Elsa Meyer
Introduction
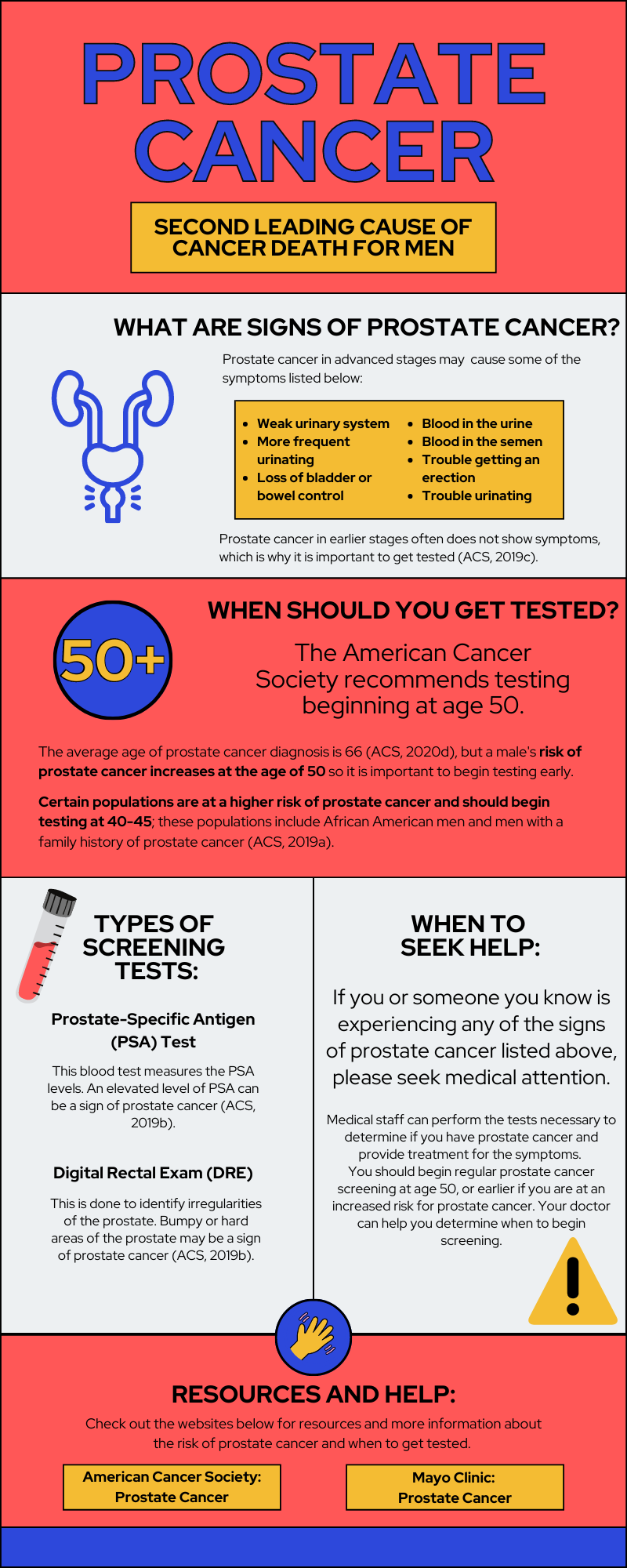
Prostate cancer occurs in the prostate gland of males. According to the American Cancer Society ([ACS] 2020d), prostate cancer is the second most common cancer for American men and about 1 in 8 men will be diagnosed with prostate cancer. One in 41 men will die from prostate cancer, making it the second leading cancer that results in death for American men. Prostate cancer typically appears in men over the age of 65 (Rawla, 2019). Most prostate cancers grow slowly and don’t affect the male for years, but some grow quickly, metastasize, or result in death (ACS, 2020d).
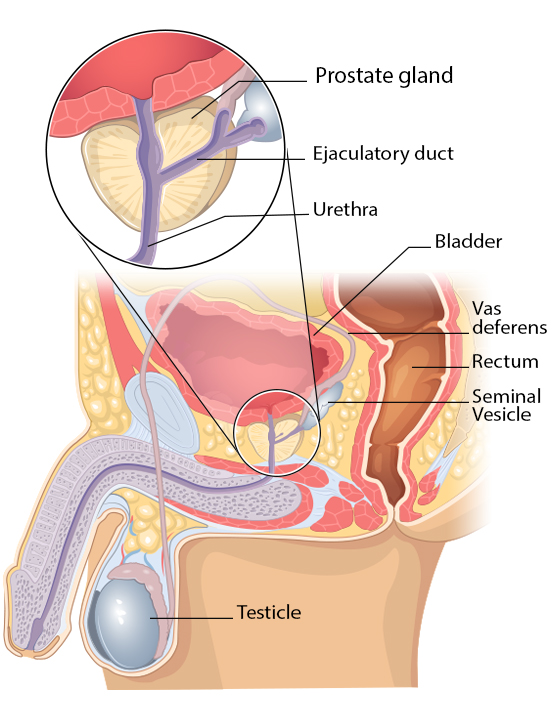
The prostate gland is a small gland that produces seminal fluid, which helps transport and provides energy to sperm. Sperm travels from the testes, through the prostate and penis, and out of the body (Prostate Cancer Foundation, n.d.).
Causes, Risk Factors, and Prevention
The main cause of prostate cancer is unknown to scientists. However, there are various risk factors and doctors have an idea of how prostate cancer develops. Cancer is caused by a mutation of DNA, which is inherited or randomly occurs (2020b). Some of the risk factors mentioned below may potentially lead to random mutations that cause prostate cancer.
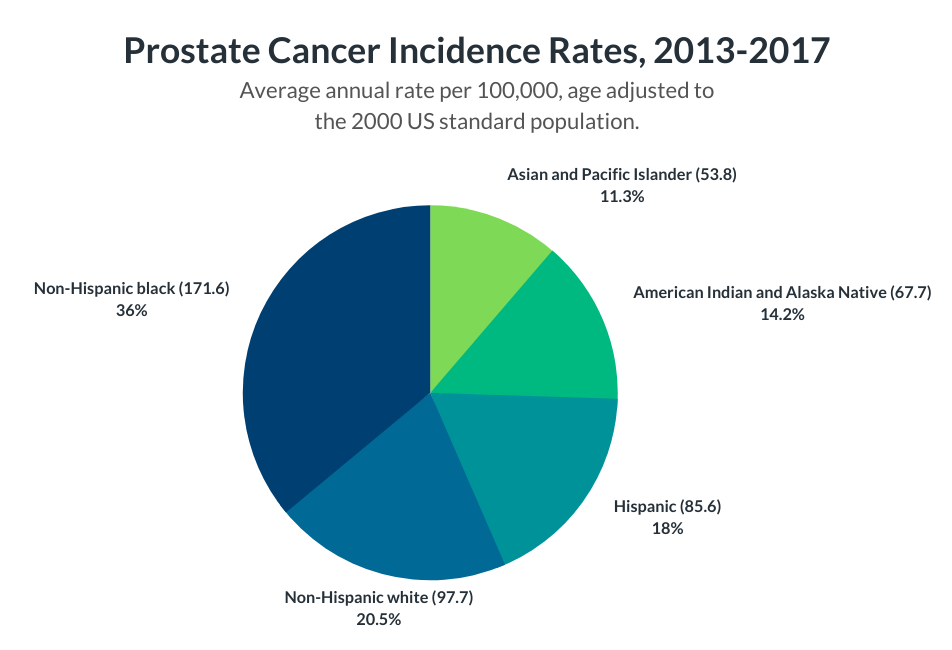
Risk factors for prostate cancer include old age, with the risk increasing at age 50 according to the Mayo Clinic (n.d.). Prostate cancer is seen more often in African-American men than any other race (ACS, 2020d). African-American men diagnosed with prostate cancer are also more likely to die from prostate cancer (Physician Data Query Screening [PDQ] and Prevention Editorial Board, 2019). More cases are seen in North America, Northwestern Europe, and Australia, and less often in Asia, Africa, and Central and South America. Some suggest this is due to higher testing and screening in these more developed areas (ACS, 2020a). Men with a family history of prostate cancer are at an increased risk, but the genetic link is unclear to scientists. Obesity is a potential risk factor and some studies have displayed a link to a higher risk of more aggressive forms of prostate cancer (ACS, 2020a; Mayo Clinic, n.d.). Other risk factors listed by the National Cancer Institute include hormones, vitamin E, folic acid, dairy, and calcium (PDQ Screening and Prevention Editorial Board, 2019). Risk factors stated by the American Cancer Society (2020a) also list smoking, chemical exposures, inflammation of the prostate, sexually transmitted infections, and vasectomies.
Because the cause of prostate cancer is largely unknown, prostate cancer prevention involves the body’s overall health. To reduce the risk of prostate cancer, the Mayo Clinic (n.d) recommends a healthy diet, frequent exercise, and maintaining a healthy weight.
Detection and Screening
Prostate cancer in the early stages doesn’t typically show symptoms, so a majority of cases are found through screening. More advanced prostate cancers show symptoms, including trouble urinating, a weak urinary stream, more frequent urinating, blood in the urine, blood in the semen, trouble getting an erection, bone pain, weakness in the legs or feet, loss of bladder or bowel control, and losing weight without trying (ACS, 2019c; Mayo Clinic, n.d.).
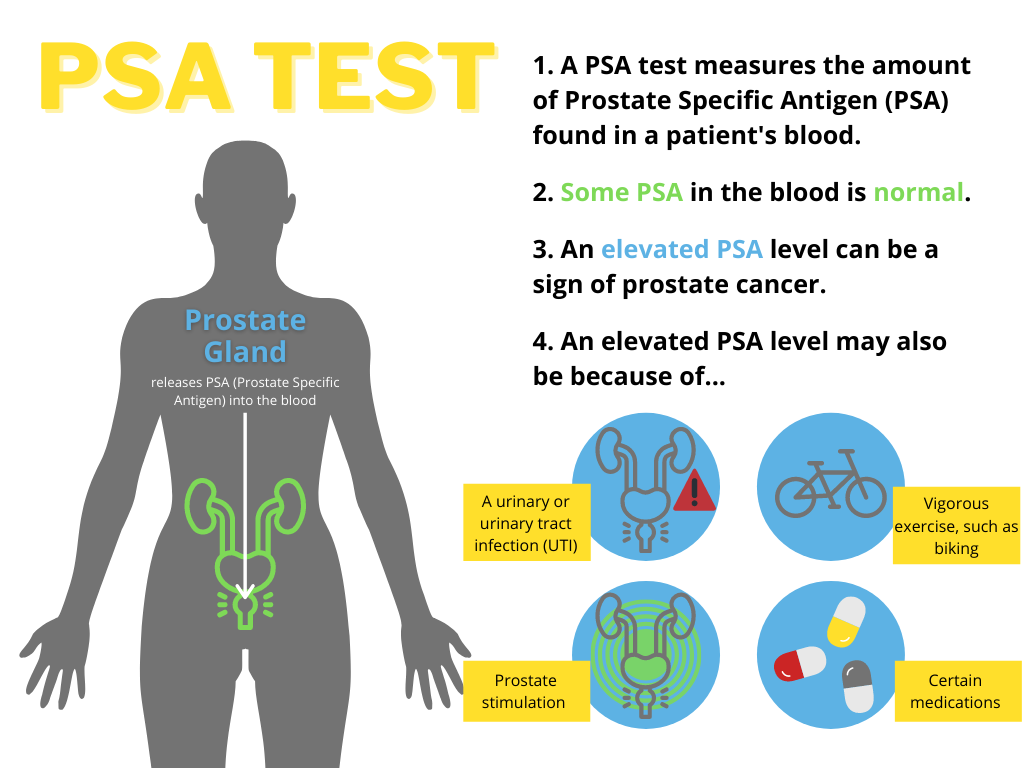
Men at average risk of prostate cancer should consider screening tests beginning at age 50 (ACS, 2019a). Rawla (2019) claims earlier screening “is highly recommended at age 45 for men with familial history and African-American men”. Prostate-specific antigen (PSA) level is tested to determine if there is an increased risk of prostate cancer. PSA levels can vary due to many factors, so it is often suggested to take another PSA test after a month if the initial PSA test showed abnormal results (ACS, 2019b).
Another screening test is the digital rectal exam (DRE), which is performed by the doctor inserting a finger into the rectum to inspect the prostate. The doctor feels for any irregular areas that may be bumpy or harder than normal. If these screening tests indicate the possibility of prostate cancer, a prostate biopsy is recommended. A biopsy takes a small sample of the prostate to be looked at under the microscope to determine if it is cancerous (ACS, 2019b).
Diagnosis and Treatment
Once a prostate biopsy is performed and cancer is found, the cancer is assigned a grade, called a Gleason score (ACS, 2019d). Two sections of the cancer are observed under a microscope and each given a score, with a lower score looking similar to healthy tissue. A higher Gleason score indicates more advanced prostate cancer (ACS, 2019d).
Prostate cancers often grow slowly and don’t pose significant, immediate health threats to the individual. Dr. Allaf (n.d.) from Johns Hopkins discusses active surveillance as an approach to these slow-growing cancers with a low risk of causing symptoms. Active surveillance could include a rectal exam and PSA test twice a year, a prostate biopsy once a year, or an MRI scan. Doctors recommend this option to cases that qualify to avoid the harsh side effects of treatment options that may harm the patient.
There are many treatment options for prostate cancer in more advanced stages. The type of treatment approach varies greatly between prostate cancer cases (ACS, 2020c). The American Cancer Society (2020c) lists surgery, radiation therapy, chemotherapy, immunotherapy, and more. Treatment effectiveness is very different for each patient, and studies have shown a variety of results but conclude that active surveillance is increasing in popularity and effectiveness (Jayadevappa et al., 2017). The infographic included below provides a summary of prostate cancer and resources to learn more.
Chapter Review Questions
1. What is the main function of the prostate gland?
A. Holds urine
B. Produces sperm
C. Produces seminal fluid
D. Makes testosterone
2. The following are signs and symptoms of prostate cancer except:
A. Blood in the urine
B. Constipation
C. Trouble urinating
D. Loss of bladder control
3. What does a high PSA level in a person’s blood indicate?
A. Increased risk of prostate cancer
B. A urinary tract infection
C. Recent prostate stimulation
D. All of the above
References
Allaf, M. E. (n.d.). Prostate cancer: When to treat versus when to watch. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/prostate-cancer-treatment-what-to-know-about-active-surveillance
American Cancer Society. (2019a, August 1). American Cancer Society recommendations for prostate cancer early detection. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/acs-recommendations.html
American Cancer Society. (2019b, August 1). Screening tests for prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/tests.html
American Cancer Society. (2019c, August 1). Signs and symptoms of prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/signs-symptoms.html
American Cancer Society. (2019d, August 1). Tests to diagnose and stage prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/how-diagnosed.html
American Cancer Society. (2020a, June 9). Prostate cancer risk factors. https://www.cancer.org/cancer/prostatecancer/causes-risks-prevention/risk-factors.html
American Cancer Society. (2020b, June 9). What causes prostate cancer? https://www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/what-causes.html
American Cancer Society. (2020c, June 11). Treating prostate cancer. https://www.cancer.org/cancer/prostatecancer/treating.html
American Cancer Society. (2020d, December 10). About prostate cancer.https://www.cancer.org/cancer/prostate-cancer/about.html
Jayadevappa, R., Chhatre, S., Wong, Y. N., Wittink, M. N., Cook, R., Morales, K. H., Vapiwala, N., Newman, D. K., Guzzo, T., Wein, A. J., Malkowicz, S. B., Lee, D. I., Schwartz, J. S., & Gallo, J. J. (2017, May). Comparative effectiveness of prostate cancer treatments for patient-centered outcomes: A systematic review and meta-analysis (PRISMA Compliant). Medicine, 96(18) e6790. https://doi.org/10.1097/MD.0000000000006790
Mayo Clinic. (n.d.). Prostate cancer. https://www.mayoclinic.org/diseases-conditions/prostate-cancer/symptoms-causes/syc-20353087
Physician Data Query Screening and Prevention Editorial Board. (2019, April 10). Physician Data Query prostate cancer screening. National Cancer Institute. https://www.cancer.gov/types/prostate/patient/prostate-screening-pdq
Prostate Cancer Foundation. (n.d.) Prostate gland. https://www.pcf.org/about-prostate-cancer/what-is-prostate-cancer/prostate-gland/
Rawla, P. (2019). Epidemiology of prostate cancer. World Journal of Oncology, 10(2), 63–89. https://doi.org/10.14740/wjon1191
spread or growth of cancer to another part of the body
a relatively permanent change in hereditary material
surgical division or resection of all or part of the vas deferens usually to induce sterility
type of cancer treatment that uses beams of intense energy to kill cancer cells
the administration of one or more cytotoxic drugs to destroy or inhibit the growth and division of malignant cells in the treatment of cancer
treatment or prevention of disease (such as an autoimmune disorder, allergy, or cancer) that involves the stimulation, enhancement, suppression, or desensitization of the immune system

