9 Testicular Torsion
David Cote
Introduction

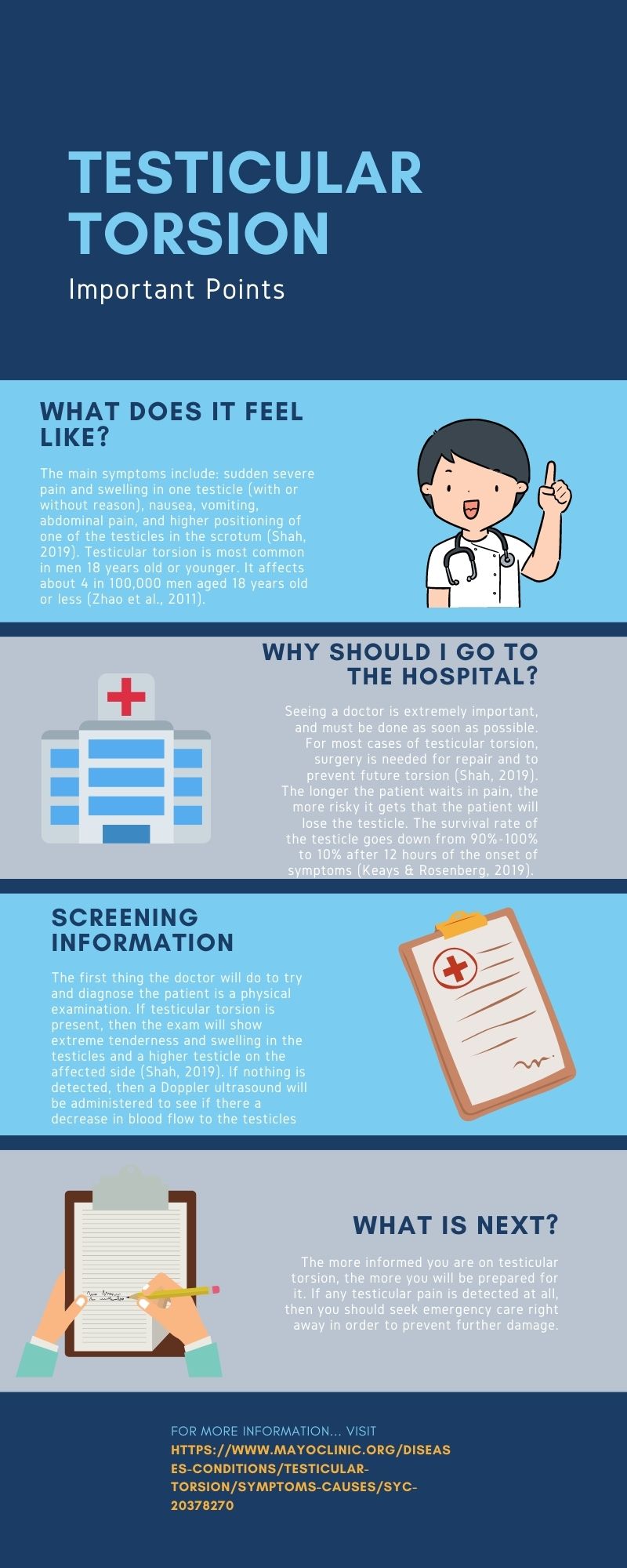
Testicular torsion occurs when the testicles rotate and the spermatic cord twists. The spermatic cord brings blood flow to the scrotum; therefore, the twisting will reduce the amount of blood getting to the scrotum, which will cause severe pain and swelling. Testicular torsion requires immediate surgical attention, and if blood flow is completely stopped, then the testicle may have to be surgically removed. It is extremely painful and permanent damage is almost certain if not treated quickly. For males younger than 18 years old, the estimated yearly frequency of testicular torsion is about 4 per 100,000 (Zhao et al., 2011). There is still no real cause for testicular torsion, although it has been found mainly in men who have an inherited trait that allows the testicle to rotate freely inside the scrotum (Mayo Foundation for Medical Education and Research, 2020). Moreover, injury to the testicles due to sports, exercise, or an accident can be associated with the onset of testicular torsion (Mayo Foundation for Medical Education and Research, 2020).
Testing
People need to seek immediate medical attention if they experience the following symptoms: severe pain or swelling in the scrotum, abdominal pain, nausea, or vomiting. One possible way for a doctor to assess if a patient has testicular torsion is through the TWIST (Testicular Workup for Ischemia and Suspected Torsion) score. The Canadian Medical Association Journal writes, “Scoring is as follows: testicular swelling (2 points), hard testis (2 points), absent cremasteric reflex (1 point), nausea and vomiting (1 point), and high-riding testis (1 point)” (Keays & Rosenberg, 2019). Scoring of 0 means that there is no indication of testicular torsion, whereas a score of 6 or 7 is highly predictive of testicular torsion. Another testing method used is an ultrasound, which can detect structural issues and the amount of blood flow to the testes (El-Feky et al., 2021). Ultrasound results can show twisting of the spermatic cord, altered blood flow, increase in the size of the testis, and thickening of the scrotal skin with hyperemia (El-Feky et al., 2021).
More Common in Boys Than Men
Testicular torsion is seen most commonly in both young adults and babies that are four weeks old or younger. Testicular torsion in young adults is more common due to the bell clapper deformity. Bell clapper deformity is something that affects the spermatic cord in such a way to allow the testis to move more freely. This occurs in 5%-16% of males and increases the risk of the spermatic cord getting twisted (El-Feky et al., 2021). One study performed by the Journal of Urology showed the distribution of testicular torsion to peak in the first year of life and early adolescence (Zhao et al., 2011). The study also revealed that orchiectomies were performed on about 42% of boys undergoing surgery for torsion. Orchiectomy rates were highest in kids younger than 10 years old, and there was an increased frequency of orchiectomy among cases in the Black race (Zhao et al., 2011). Since this is an irregular condition, there is no difference in saving the testicle among different races (Ramachandra et al., 2015).
Repair and Future Effects
Surgery is the only practical option for a patient with twisted testicles in order to save the testicles. In order to perform the surgery, the surgeon will cut the scrotum to gain access to the twisted spermatic cord. The cord will be untwisted, and then the surgeon will stitch the testicle to the scrotum. The surgeon will do this to both testicles to prevent future problems by not allowing the testicles to move freely inside the sac. If one testicle has to be removed, the other testicle should be able to provide enough hormones for male growth, sex life, and fertility (Shah, 2019). When surgical correction is performed within 6 hours of the start of testicular torsion, there is 90%-100% survival rate of the testicle. However, when surgery is performed within 12-24 hours from the start of testicular torsion, there is only 10% survival rate of the testicle (Keays & Rosenberg, 2019). Although more research needs to be done, there is some notice of lower sperm quality after testicular torsion. Moreover, animal studies have demonstrated testicular torsion’s negative impact on the testis opposite of the twisted testis. The impact is due to blood supply returning rapidly after a period of absence of oxygen (Jacobsen et al., 2020).
Prevention
Although there is no clear prevention for testicular torsion besides surgery, awareness of it can help to avoid permanent damage. A study done by Children’s Health (n.d.) found that males under 18 years old waited up to 20 hours before going to the emergency room. Although it may be uncomfortable to talk to a parent about genital problems, boys need to speak up to prevent further problems in the future. Also, it could never hurt to wear proper protection during sports in order to prevent direct contact with the testicles. However, the only true way to stop future testicular torsion is by stitching the testicle to the scrotum through testicular torsion repair surgery.
Summary of Testicular Torsion
Chapter Review Questions
1. What is the only actual way to prevent testicular torsion from occurring?
A. There is no way to prevent testicular torsion
B. Stitching the testicle to the scrotum through surgery
C. Exercising on a daily basis
D. Massaging the testicle to increase blood flow
2. What is the survival rate of a testicle when surgery is performed within 12-24 hours from the onset of testicular torsion?
A. 90%
B. 50%
C. 10%
D. 42%
3. Which of the following symptoms is concurrent with testicular torsion?
A. Difficulty urinating
B. High fever
C. Intense itching of the groin
D. Abdominal pain
References
El-Feky, M., Gaillard, F., & Hacking, C. (2021, April 13). Testicular torsion. Radiopaedia. https://radiopaedia.org/articles/testicular-torsion
Jacobsen, F. M., Rudlang, T. M., Fode, M., Østergren, P.,B., Sønksen, J., Ohl, D. A., Jensen, C. F. S., & Collaborative, C. (2020). The impact of testicular torsion on testicular function. The World Journal of Men’s Health, 38(3), 298-307. 10.5534/wjmh.190037
Keays, M., & Rosenberg, H. (2019). Testicular torsion. CMAJ: Canadian Medical Association Journal, 191(28), E792. 10.1503/cmaj.190158
Mayo Foundation for Medical Education and Research. (2020, April 4). Testicular torsion. Mayo clinic. https://www.mayoclinic.org/diseases-conditions/testicular-torsion/symptoms-causes/syc-20378270
Ramachandra, P., Palazzi, K. L., Holmes, N. M., & Marietti, S. (2015). Factors influencing rate of testicular salvage in acute testicular torsion at a tertiary pediatric center. The Western Journal of Emergency Medicine, 16(1), 190-194. 10.5811/westjem.2014.11.22495
Shah, S. M. (2019, July 31). Testicular torsion repair. MedlinePlus. https://medlineplus.gov/ency/article/002994.htm
Children’s Health. (n.d.). Testicular torsion: Signs, causes and what to do. https://www.childrens.com/health-wellness/testicular-torsion-signs-causes-what-to-do.
Zhao, L. C., Lautz, T. B., Meeks, J. J., & Maizels, M. (2011). Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. The Journal of Urology, 186(5), 2009-2013. 10.1016/j.juro.2011.07.024
a pouch of skin containing the testicles
a restriction in blood supply to tissues, causing a shortage of oxygen that is needed for cellular metabolism
absence of the contraction of the ipsilateral cremaster muscle, drawing the testis upward, when the upper inner aspect of the thigh is stroked longitudinally
A type of imaging test to examine the internal organs using very high frequency sound waves
an excess of blood in the vessels supplying an organ or other part of the body
Surgical removal of one or both testicles

