Hannah Fortune
Introduction
In males, there are a few different kinds of hormones. The main type that most everyone knows about is testosterone. However, males actually also have the female hormone, estrogen. The types of estrogen that men have are called estrone and estradiol (Jewell, 2019). Men also have the androgens DHEA and androstenedione (Gray et al., 2017). It is important for men to understand the roles of these hormones as they age.
Hormone Production
Testosterone is produced in a couple of different places in the body. The main place is the Leydig cells, found in the testes. The adrenal glands also produce a small amount of testosterone. Testosterone production is regulated by certain areas of the brain, the hypothalamus, and the pituitary gland. The hypothalamus releases a hormone called gonadotropin-releasing hormone, which makes the pituitary gland produce and release another hormone called luteinizing hormone (LH). Once LH enters the bloodstream, it travels to the testes and starts the production of testosterone (Society for Endocrinology, 2018). Estrogen is also produced in different places in the male body. The testes produce around 20% of a male’s total estrogen, while the rest actually comes from the conversion of testosterone in areas of the body such as fat tissue, bones, the skin, and the brain (Cooke et al., 2017).
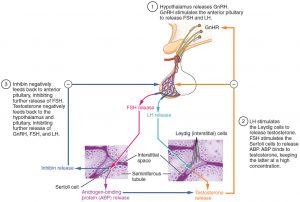 File:Figure 28 01 07.JPG by Wikimedia Commons is licensed under CC BY 3.0
File:Figure 28 01 07.JPG by Wikimedia Commons is licensed under CC BY 3.0
Role of Testosterone
Testosterone plays a very important role in many different ways throughout a male’s life. For instance, it helps with the development of male reproductive organs before birth, contributes to men’s voices getting deeper and the presence of facial hair and acne during puberty, it gives muscles their size and strength, and it helps with a male’s libido, or sex drive (Harvard Health Publishing Harvard Medical School, 2019). When a male has too much testosterone, it can lead to many problems. Some of these problems include low sperm count and smaller testicles, increased risk of heart attacks, liver disease, acne, weight gain, high blood pressure, and high cholesterol (Harvard Health Publishing Harvard Medical School, 2019). Not having enough testosterone leads to its own health problems which can include less hair, loss of bone density and muscle mass, low sex drive, and a low sperm count (Harvard Health Publishing Harvard Medical School, 2019). Reproductive organ problems, along with genetic diseases such as Klinefelter syndrome and hemochromatosis can cause issues with testosterone levels in a male’s body (Harvard Health Publishing Harvard Medical School, 2019).
Role of Estrogen
Interestingly enough, estrogen plays a pretty important role in the male body. Estrogen works along with testosterone to help manage sex drive, erectile function, and sperm production (Jewell, 2019). Just like with testosterone, when a male has too much or too little estrogen, health problems can occur. If a male has too much estrogen, they can experience infertility, erectile dysfunction, slow growth during puberty, an increase in breast fat tissue, and reduced sperm count. If a male does not have enough estrogen not many side effects occur; however, have hormone levels tested regularly in case men need to get treated to get it under control (Jewell, 2019). As men age, their testosterone levels decrease, but their estrogen levels actually increase (Jewell, 2019).
Effects on Behavior
Testosterone has been found to have an effect on behavior throughout a male’s life. It has become apparent that exposure to male-related hormones before birth has an effect on a male’s gender identity and gender-based interests when they are a child (Gray et al., 2017). Before puberty is reached, these hormones play a role in helping males learn skills that will prepare them for future competition with other males (Gray et al., 2017). High levels of testosterone can lead to feelings of anger and aggression. There is evidence that testosterone levels are higher in people who commonly display excessive aggression, such as prisoners whose crimes were violent (Batrinos, 2012).
Testosterone Therapy
The purpose of testosterone therapy is to improve a male’s quality of life or health if his testosterone levels are too low. Despite this, testosterone therapy is a very controversial subject. Therapy benefits may include improvement in energy, sex drive, muscle mass, insulin resistance, and bone mineral density (Khera, 2016). However, short-term side effects could be acne, sleep apnea, swelling or tenderness in the breasts, and swelling in the ankles, although these effects are not extremely common. In the long-term, men who use testosterone therapy have an increased risk of developing cardiovascular issues, and some doctors worry that therapy can stimulate oncogenes for prostate cancer specifically (Harvard Health Publishing Harvard Medical School, 2020).
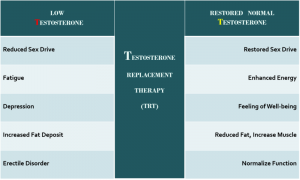
File: Symptoms of Low-T & and TRT to restore.png by Wikimedia Commons is licensed under CC BY-SA 4.0
When to Seek Help
If a male begins to notice acne or weight gain, they may be producing too much testosterone. If hair loss, loss of muscle mass, and reduced sex drive begin occurring, too little testosterone is being produced. Lastly, if a male notices an increase in breast tissue, erectile dysfunction, or that they are growing too slowly, they are producing too much estrogen. All of these are signs of an imbalance in the hormones and should be checked out by a doctor to prevent any long-term damage.

Chapter Review Questions
1. What role does testosterone play before a male is born?
A. Produces body hair
B. Develops the reproductive organs
C. Gives muscles size and strength
D. Contributes to the deepening of the voice
2. Where is the majority of a male’s testosterone produced?
A. Adrenal glands
B. The penis
C. Leydig cells
D. Adrenal gland
3. What percent of a male’s total estrogen do the testes produce?
A. 20%
B. 25%
C. 50%
D. 80%
References
Batrinos, M. L., (2012). Testosterone and aggressive behavior in man. International Journal of Endocrinology and Metabolism, 10(3), 563-568. 10.5812/ijem.3661
Cooke, P. S., Nanjappa, M. K., Ko, C., Prins, G. S., & Hess, R. A. (2017). Estrogens in male physiology. Physiological Reviews, 97(3), 995-1043. 10.1152/physrev.00018.2016
Gray, P. B., McHale, T. S., & Carré, J. M. (2017). A review of human male field studies of hormones and behavioral reproductive effort. Hormones and Behavior, 91, 52-67. 10.1016/j.yhbeh.2016.07.004
Harvard Health Publishing Harvard Medical School. (2020, August 19). Is testosterone therapy safe? Take a breath before you take the plunge. https://www.health.harvard.edu/mens-health/is-testosterone-therapy-safe-take-a-breath-before-you-take-the-plunge
Harvard Health Publishing Harvard Medical School (2019, August 29). Testosterone-What it does and doesn’t do. https://www.health.harvard.edu/drugs-and-medications/testosterone–what-it-does-and-doesnt-do
Jewell, T., (2019, October 22). Risk factors of having high or low estrogen levels in males. Healthline. https://www.healthline.com/health/estrogen-in-men
Khera, M., (2016). Male hormones and men’s quality of life. Current Opinion in Urology, 26(2), 152-157. 10.1097/MOU.0000000000000256.
Lopez, D., Peskoe, S., Joshu, C., Dobs, A., Feinleib, M., Kanarek, N., Nelson, W., Selvin, E., Rohrmann, S., & Platz, E. (2013). Racial/ethnic differences in serum sex steroid hormone concentrations in US adolescent males. Cancer Causes & Control, 24 (4) 817–826. 10.1007/s10552-013-0154-8
Society for Endocrinology. (2018, February). Testosterone. You and your hormones. https://www.yourhormones.info/hormones/testosterone/
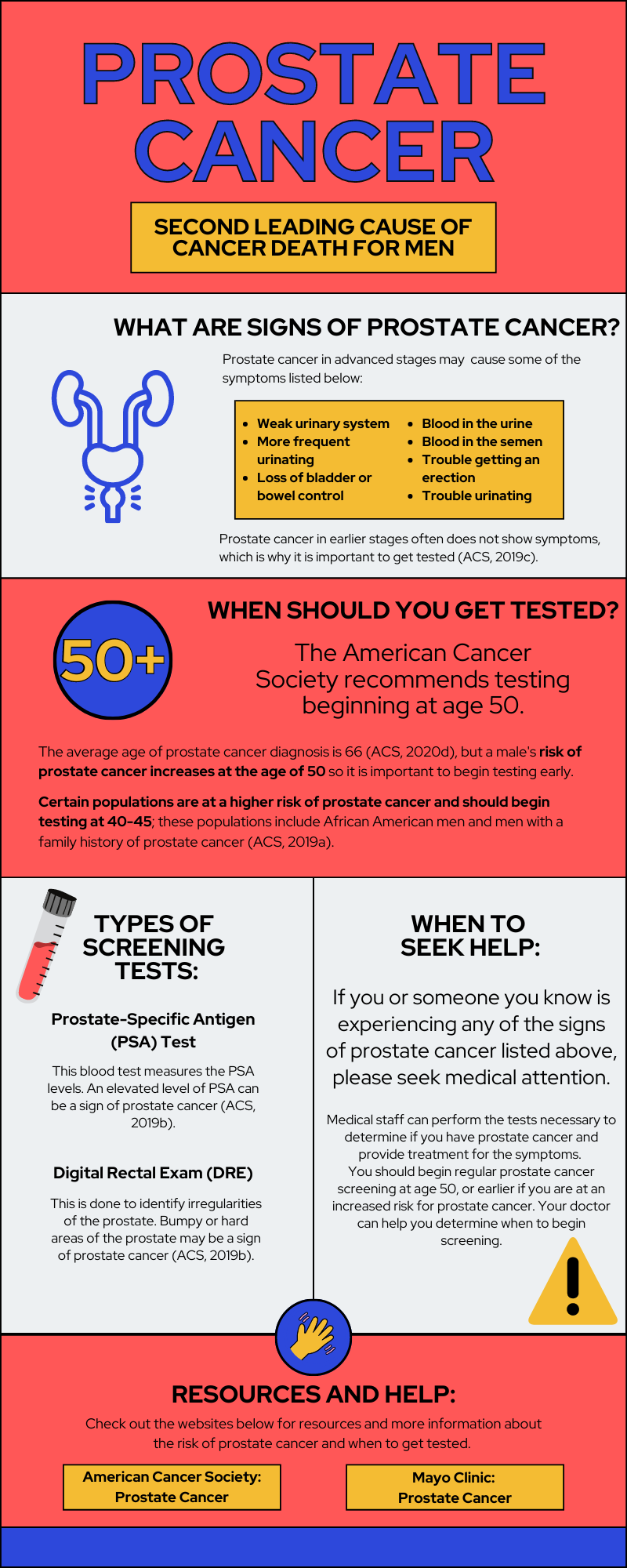
Introduction
Prostate cancer occurs in the prostate gland of males. According to the American Cancer Society ([ACS] 2020d), prostate cancer is the second most common cancer for American men and about 1 in 8 men will be diagnosed with prostate cancer. One in 41 men will die from prostate cancer, making it the second leading cancer that results in death for American men. Prostate cancer typically appears in men over the age of 65 (Rawla, 2019). Most prostate cancers grow slowly and don’t affect the male for years, but some grow quickly, metastasize, or result in death (ACS, 2020d).
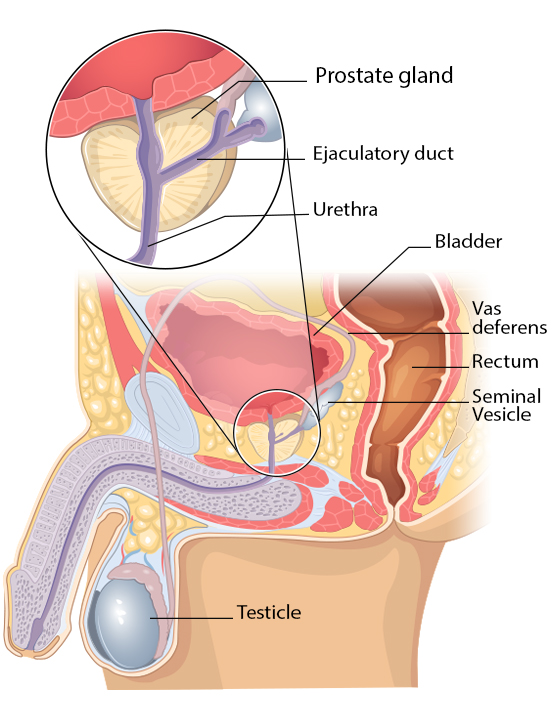
The prostate gland is a small gland that produces seminal fluid, which helps transport and provides energy to sperm. Sperm travels from the testes, through the prostate and penis, and out of the body (Prostate Cancer Foundation, n.d.).
Causes, Risk Factors, and Prevention
The main cause of prostate cancer is unknown to scientists. However, there are various risk factors and doctors have an idea of how prostate cancer develops. Cancer is caused by a mutation of DNA, which is inherited or randomly occurs (2020b). Some of the risk factors mentioned below may potentially lead to random mutations that cause prostate cancer.
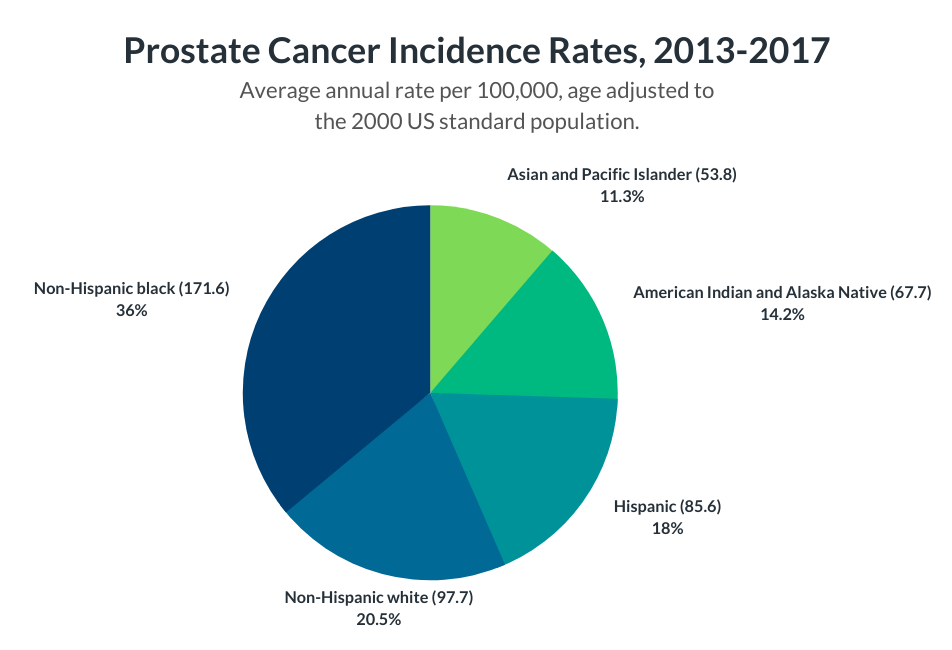
Risk factors for prostate cancer include old age, with the risk increasing at age 50 according to the Mayo Clinic (n.d.). Prostate cancer is seen more often in African-American men than any other race (ACS, 2020d). African-American men diagnosed with prostate cancer are also more likely to die from prostate cancer (Physician Data Query Screening [PDQ] and Prevention Editorial Board, 2019). More cases are seen in North America, Northwestern Europe, and Australia, and less often in Asia, Africa, and Central and South America. Some suggest this is due to higher testing and screening in these more developed areas (ACS, 2020a). Men with a family history of prostate cancer are at an increased risk, but the genetic link is unclear to scientists. Obesity is a potential risk factor and some studies have displayed a link to a higher risk of more aggressive forms of prostate cancer (ACS, 2020a; Mayo Clinic, n.d.). Other risk factors listed by the National Cancer Institute include hormones, vitamin E, folic acid, dairy, and calcium (PDQ Screening and Prevention Editorial Board, 2019). Risk factors stated by the American Cancer Society (2020a) also list smoking, chemical exposures, inflammation of the prostate, sexually transmitted infections, and vasectomies.
Because the cause of prostate cancer is largely unknown, prostate cancer prevention involves the body's overall health. To reduce the risk of prostate cancer, the Mayo Clinic (n.d) recommends a healthy diet, frequent exercise, and maintaining a healthy weight.
Detection and Screening
Prostate cancer in the early stages doesn’t typically show symptoms, so a majority of cases are found through screening. More advanced prostate cancers show symptoms, including trouble urinating, a weak urinary stream, more frequent urinating, blood in the urine, blood in the semen, trouble getting an erection, bone pain, weakness in the legs or feet, loss of bladder or bowel control, and losing weight without trying (ACS, 2019c; Mayo Clinic, n.d.).
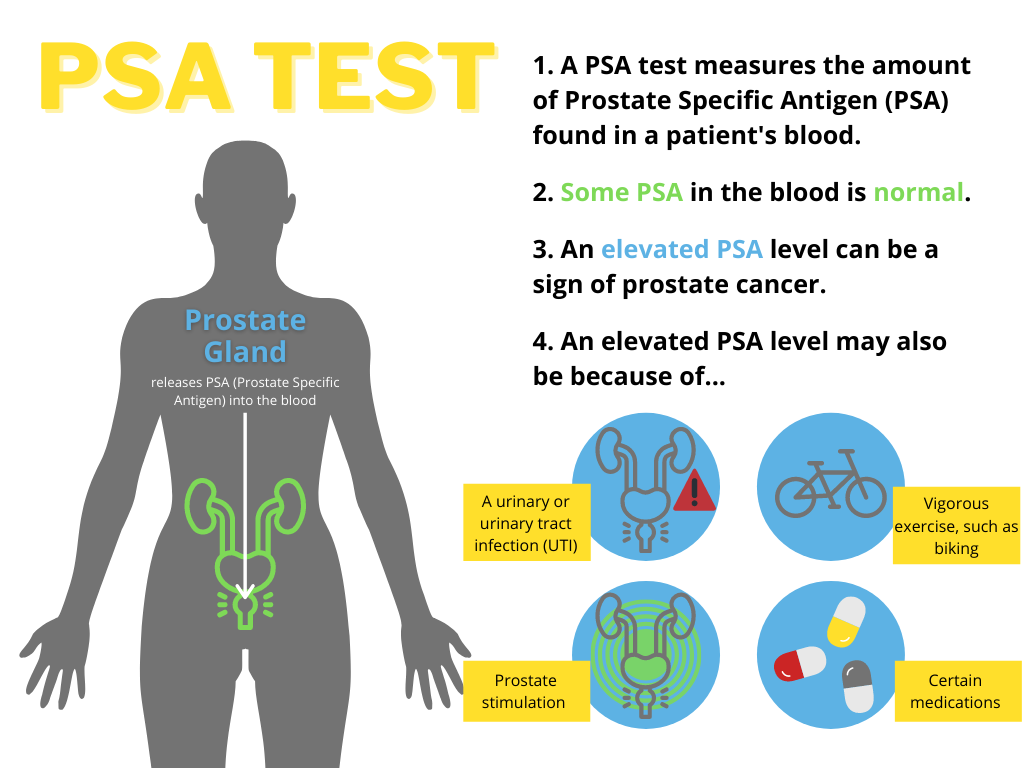
Men at average risk of prostate cancer should consider screening tests beginning at age 50 (ACS, 2019a). Rawla (2019) claims earlier screening “is highly recommended at age 45 for men with familial history and African-American men”. Prostate-specific antigen (PSA) level is tested to determine if there is an increased risk of prostate cancer. PSA levels can vary due to many factors, so it is often suggested to take another PSA test after a month if the initial PSA test showed abnormal results (ACS, 2019b).
Another screening test is the digital rectal exam (DRE), which is performed by the doctor inserting a finger into the rectum to inspect the prostate. The doctor feels for any irregular areas that may be bumpy or harder than normal. If these screening tests indicate the possibility of prostate cancer, a prostate biopsy is recommended. A biopsy takes a small sample of the prostate to be looked at under the microscope to determine if it is cancerous (ACS, 2019b).
Diagnosis and Treatment
Once a prostate biopsy is performed and cancer is found, the cancer is assigned a grade, called a Gleason score (ACS, 2019d). Two sections of the cancer are observed under a microscope and each given a score, with a lower score looking similar to healthy tissue. A higher Gleason score indicates more advanced prostate cancer (ACS, 2019d).
Prostate cancers often grow slowly and don’t pose significant, immediate health threats to the individual. Dr. Allaf (n.d.) from Johns Hopkins discusses active surveillance as an approach to these slow-growing cancers with a low risk of causing symptoms. Active surveillance could include a rectal exam and PSA test twice a year, a prostate biopsy once a year, or an MRI scan. Doctors recommend this option to cases that qualify to avoid the harsh side effects of treatment options that may harm the patient.
There are many treatment options for prostate cancer in more advanced stages. The type of treatment approach varies greatly between prostate cancer cases (ACS, 2020c). The American Cancer Society (2020c) lists surgery, radiation therapy, chemotherapy, immunotherapy, and more. Treatment effectiveness is very different for each patient, and studies have shown a variety of results but conclude that active surveillance is increasing in popularity and effectiveness (Jayadevappa et al., 2017). The infographic included below provides a summary of prostate cancer and resources to learn more.
Chapter Review Questions
1. What is the main function of the prostate gland?
A. Holds urine
B. Produces sperm
C. Produces seminal fluid
D. Makes testosterone
2. The following are signs and symptoms of prostate cancer except:
A. Blood in the urine
B. Constipation
C. Trouble urinating
D. Loss of bladder control
3. What does a high PSA level in a person’s blood indicate?
A. Increased risk of prostate cancer
B. A urinary tract infection
C. Recent prostate stimulation
D. All of the above
References
Allaf, M. E. (n.d.). Prostate cancer: When to treat versus when to watch. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/prostate-cancer-treatment-what-to-know-about-active-surveillance
American Cancer Society. (2019a, August 1). American Cancer Society recommendations for prostate cancer early detection. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/acs-recommendations.html
American Cancer Society. (2019b, August 1). Screening tests for prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/tests.html
American Cancer Society. (2019c, August 1). Signs and symptoms of prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/signs-symptoms.html
American Cancer Society. (2019d, August 1). Tests to diagnose and stage prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/how-diagnosed.html
American Cancer Society. (2020a, June 9). Prostate cancer risk factors. https://www.cancer.org/cancer/prostatecancer/causes-risks-prevention/risk-factors.html
American Cancer Society. (2020b, June 9). What causes prostate cancer? https://www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/what-causes.html
American Cancer Society. (2020c, June 11). Treating prostate cancer. https://www.cancer.org/cancer/prostatecancer/treating.html
American Cancer Society. (2020d, December 10). About prostate cancer.https://www.cancer.org/cancer/prostate-cancer/about.html
Jayadevappa, R., Chhatre, S., Wong, Y. N., Wittink, M. N., Cook, R., Morales, K. H., Vapiwala, N., Newman, D. K., Guzzo, T., Wein, A. J., Malkowicz, S. B., Lee, D. I., Schwartz, J. S., & Gallo, J. J. (2017, May). Comparative effectiveness of prostate cancer treatments for patient-centered outcomes: A systematic review and meta-analysis (PRISMA Compliant). Medicine, 96(18) e6790. https://doi.org/10.1097/MD.0000000000006790
Mayo Clinic. (n.d.). Prostate cancer. https://www.mayoclinic.org/diseases-conditions/prostate-cancer/symptoms-causes/syc-20353087
Physician Data Query Screening and Prevention Editorial Board. (2019, April 10). Physician Data Query prostate cancer screening. National Cancer Institute. https://www.cancer.gov/types/prostate/patient/prostate-screening-pdq
Prostate Cancer Foundation. (n.d.) Prostate gland. https://www.pcf.org/about-prostate-cancer/what-is-prostate-cancer/prostate-gland/
Rawla, P. (2019). Epidemiology of prostate cancer. World Journal of Oncology, 10(2), 63–89. https://doi.org/10.14740/wjon1191
Introduction
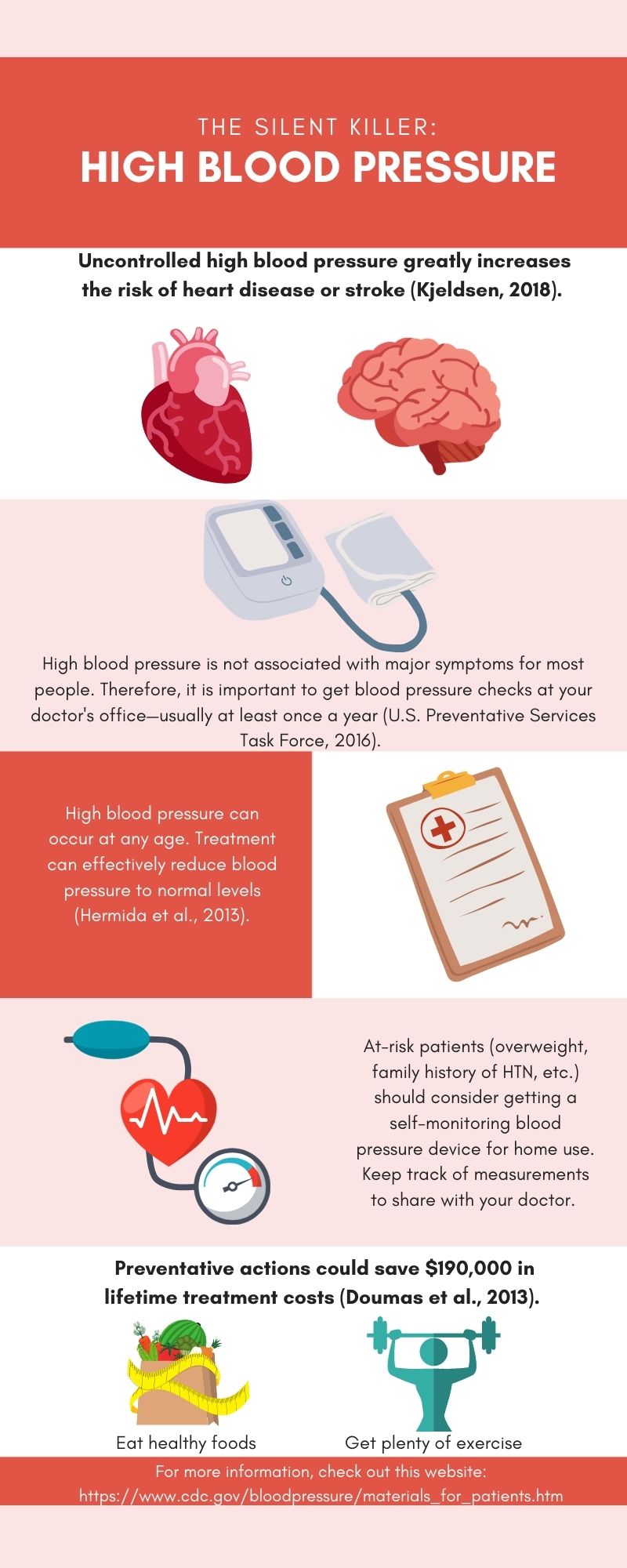
High blood pressure, or hypertension (HTN), is a major problem in the U.S. Currently, 108 million U.S. adults (50%) have been diagnosed with it, and only about 25% have it under control (Centers for Disease Control and Prevention [CDC], 2020). If not successfully managed, HTN is very dangerous, leading to heart disease or stroke (Kjeldsen, 2018). Indeed, in 2019 HTN contributed to nearly 500,000 deaths in the U.S. (CDC, 2020). While the risk of developing this disease increases with age, college-aged men are also affected (Kjeldsen 2018). A recent study showed that 27% of men in their twenties were hypertensive (Everett & Zajacova, 2015). Therefore, it is crucial for college-aged men to be informed and take preventative actions early in life.
What is High Blood Pressure?
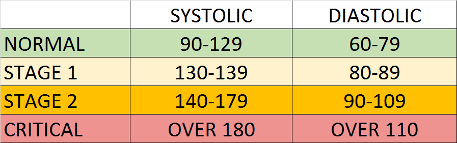
Blood pressure is the pressure that blood puts on the blood vessel walls. If blood pressure is constantly high, it can cause damage to these vessels and promote cardiovascular problems (Stevens et al., 2016). There are four blood pressure categories: normal, stage 1, stage 2, and critical (see figure). Blood pressure is measured by the systolic pressure (first or top number) and diastolic pressure (second or bottom number). Specifically, HTN is defined as blood pressure higher than 130/80 mm Hg. Typically, an HTN diagnosis is made by health professionals after several measurements over a period of time. As blood pressure increases, the risk of a sudden heart attack or stroke increases dramatically. Therefore, it is important to keep blood pressure under control.
There are two main categories of HTN: essential (also known as primary) and secondary. The majority of patients (95-98%) have essential HTN. For this type, there is no single identifiable cause of the disease, but rather multiple interrelated causes (Beevers et al., 2001). It is most likely that the majority of college-aged males with HTN would fall in the essential HTN group. Secondary HTN, which only 2-5% of patients have, is classified as HTN due to an underlying kidney or adrenal gland disease.
HTN prevalence varies between males and females depending on age. Generally, more men have HTN than women, but there is not always a major difference. Recent data from 2015-2018 showed that in the U.S., more men have HTN up to age 64, but more women have HTN after age 64 (Virani et al., 2020). There are several reasons for the observed age and gender differences in HTN prevalence. One reason is that women are more protected because of the effects of estrogens before menopause. However, other reasons could be due to differences in salt sensitivity between men and women or that men have an increased likelihood of developing problems with their hearts (Doumas et al., 2013).
High Blood Pressure Awareness and Treatment

High blood pressure is often known as the “silent killer” because it is not associated with major symptoms. Many people, including college-aged men, do not even realize they have HTN. A 2015 study found that only 25% of men in their twenties were aware of their hypertensive status (Everett & Zajacova, 2015). Therefore, it is important to get regular blood pressure checks to screen for HTN. It is recommended that adults 18 years or older with normal blood pressure and no risk factors be rescreened every 3-5 years. However, adults ≥40 years old or persons at an increased risk for HTN should be rescreened annually (United States Preventative Services Task Force, 2016). Several studies have shown that treatment can effectively reduce HTN (Hermida et al., 2013). Unfortunately, less than 50% of people (mostly ≤40 years old) continue to take their medications after one year (Burnier & Egan, 2019). These statistics are mainly due to the perceived side effects of the medications. However, it is best to discuss other treatment methods with a physician rather than having no treatment at all.
Preventing High Blood Pressure
There are many steps men can take to reduce the risk of developing HTN. First, it is essential to eat healthy foods and get plenty of exercise. It has been found that proper diet and exercise (both aerobic and strength training) are effective at lowering high blood pressure (Jurik & Stastny, 2019). Additionally, there is some evidence that high sodium intake raises blood pressure (He et al., 2012). It is estimated that the average American eats close to 1,000 mg over the recommended sodium intake levels (Strazzullo & Leclercq, 2014). Therefore, it is best to eat fresh produce and minimize large quantities of high-sodium packaged foods.
Conclusion
Overall, it is crucial for men to understand this disease at an early age. Early preventative measures could save men $190,000, which is the average lifetime cost of HTN treatment (Doumas et al., 2013). While HTN is widespread, new technologies are improving HTN treatment. Smartphones and wearable Bluetooth blood pressure measuring devices are becoming increasingly common in HTN management. It is expected that these technologies will continue to develop and can support people with active lifestyles (Kitt et al., 2019). Although treatment is improving, college-aged men should continue to treat this disease seriously, maintain a healthy lifestyle, and educate peers on the dangers of this silent killer.
Chapter Review Questions
1. Which of the following blood pressure measurements are in the critical range?
A. 95/65 mm Hg
B. 120/80 mm Hg
C. 150/90 mm Hg
D. 190/115 mm Hg
2. Which condition is most associated with hypertension?
A. Kidney stones
B. Stroke
C. Lung cancer
D. Sickle cell anemia
3. Why is hypertension known as the silent killer?
A. Patients do not talk about the disease
B. It does not cause major symptoms
C. Doctors cannot hear blood flow
D. It is an infectious disease
References
Beevers, G., Lip, G. Y. H., & O'Brien, E. (2001). The pathophysiology of hypertension. BMJ: British Medical Journal, 322(7291), 912-916. 10.1136/bmj.322.7291.912
Burnier, M., & Egan, B. M. (2019). Adherence in hypertension: A review of prevalence, risk factors, impact, and management. Circulation Research, 124(7), 1124–1140. 10.1161/CIRCRESAHA.118.313220
Centers for Disease Control and Prevention. (2020, September 8). Facts about hypertension. https://www.cdc.gov/bloodpressure/facts.htm
Doumas, M., Papademetriou, V., Faselis, C., & Kokkinos, P. (2013). Gender differences in hypertension: myths and reality. Current Hypertension Reports, 15(4), 321–330. 10.1007/s11906-013-0359-y
Everett, B., & Zajacova, A. (2015). Gender differences in hypertension and hypertension awareness among young adults. Biodemography and Social Biology, 61(1), 1-17. 10.1080/19485565.2014.929488
He, F. J., Campbell, N. R., & MacGregor, G. A. (2012). Reducing salt intake to prevent hypertension and cardiovascular disease. Revista Panamericana de Salud Pública, 32(4), 293–300. 10.1590/s1020-49892012001000008
Hermida, R. C., Ayala, D. E., Mojon, A., & Fernández, J. R. (2013). Cardiovascular risk of essential hypertension: Influence of class, number, and treatment-time regimen of hypertension medications. Chronobiology International, 30(1–2), 315–327. 10.3109/07420528.2012.701534
Jurik, R., & Stastny, P. (2019). Role of nutrition and exercise programs in reducing blood pressure: A systematic review. Journal of Clinical Medicine, 8(9), 1393. 10.3390/jcm8091393
Kitt, J., Fox, R., Tucker, K. L., & McManus, R. J. (2019). New approaches in hypertension management: A review of current and developing technologies and their potential impact on hypertension care. Current Hypertension Reports, 21(6), 44. 10.1007/s11906-019-0949-4
Kjeldsen, S. E. (2018). Hypertension and cardiovascular risk: General aspects. Pharmacological Research, 129, 95–99. 10.1016/j.phrs.2017.11.003
Strazzullo, P., & Leclercq, C. (2014). Sodium. Advances in Nutrition, 5(2), 188–190. https://doi.org/10.3945/an.113.005215
Stevens, S. L., Wood, S., Koshiaris, C., Law, K., Glasziou, P., Stevens, R. J., & McManus, R. J. (2016). Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. British Medical Journal, 354., i4098. 10.1136/bmj.i4098
United States Preventative Services Task Force. (2016). Screening for high blood pressure in adults: recommendation statement. American Family Physician, 93(4), 300-302. https://www.aafp.org/afp/2016/0215/p300.html
Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., Chamberlain, A. M., Chang, A. R., Cheng, S., & Delling, F. N. (2020). Heart disease and stroke statistics—2020 update: A report from the American Heart Association. Circulation, 141(9), e139–e596. 10.1161/cir.0000000000000757
Whelton, P., Carey, R., Aronow, W., Casey, D., Collins, K., Dennison, H., DePalma, S., Gidding, S., Jamerson, K., Jones, D., MacLaughlin, E., Muntner, P., Ovbiagele, B., Smith, S., Spencer, C., Stafford, R., Taler, S., Thomas, R., Williams, K., … Wright, J. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension, 71(6), e13–e115. 10.1161/HYP.0000000000000066
A chronic functional disorder of the colon that is characterized especially by constipation or diarrhea, cramping abdominal pain, and the passage of mucus in the stool.

