Health and Medicine
98 Tuberculosis in America
Meghan Gamble; Kennedy Key; and Alexis Vaka
introduction
Tuberculosis, a highly variable communicable disease of humans that affects the lungs, shook 20th century America to the core. “In 1900, 194 of every 100,000 U.S. residents died from TB; most were residents of urban areas, and later in 1940, TB remained a leading cause of death” (Achievements in Public Health, 1999). As society continued without a cure throughout the 20th century, the death toll was compounding. Until the breakthrough discovery in the science of vaccinations and antibiotics, extensive and invasive treatments were utilized, often with low success rates. But when Robert Koch discovered the cause of tuberculosis and Selman Waksman developed antibiotics to combat it, the course of the disease changed forever. Innovation within science and technology to combat tuberculosis spurred the field of medicine to improve the course of public health into the future.
Background
Prior to the discovery of antibiotics for the treatment of Tuberculosis, multiple treatments, some extreme, were considered the best options for combating the disease. The formation of tuberculosis sanitariums, the artificial pneumothorax, and thoracoplasty were all commonly utilized treatments prior to the discovery of antibiotic therapies (Hurt, 2004, section 1945). Among home therapy, sanitarium quarantine was one of the most commonly prescribed treat-

ments. It was believed that the rest and environment of an isolated area within sanitariums would slow the effects of the disease and prevent it from further spreading to society (Hurt, 2004, section 1945). Ambulant patients, those who were close to being cured, were housed in open-air cottages, with the remainder of patients in the sanitarium under full or partial bed rest treatment until they were strong enough to be moved to the cottages (University of Virginia Historical Collections at the Claude Moore Health Sciences Library, 2007). While bed and cottage treatment had little measurable influence on the progression of tuberculosis, and was deemed “the alternative in a desperate search for the cure” (Ibid, pg 1) the primary use of fresh air and complete or partial immobility as a cure for disease shows the progression of tuberculosis therapy over time. Until scientifically proven treatments for Tuberculosis were formulated, such as Waksman’s streptomycin, society was confined to remedies of hope and rest as they waited for a cure to this deadly illness.
Within sanitariums, doctors performed surgeries, some extreme, for the health and welfare of patients. Two of the most commonly utilized surgeries for lung rest were the thoracoplasty and the artificial pneumothorax. The thoracoplasty involves removing ribs in a patient to reduce the volume of the lung. The compression of the lung causes cavities in lung tissue, formed by the disease, to retract and have the potential to close (Sellors, 1947). This practice, which is incredibly invasive and minimally reversible, has been proven to cause some regeneration of tissue, but has rarely resulted in complete healing of the cavities and an average of 11.4% of patients dying after the procedure, 2.7% within 4 months of surgery (Sellors, 1947). Another commonly used practice, introduced by Carlo Forlanini in 1771, the artificial pneumothorax, involves directly affecting the lung. When an artificial pneumothorax is preformed, nitrogen or oxygen gas is “I am going to peer into the field of the future therapy of pulmonary tuberculosis as an explorer, with an unsafe base of operations in an unknown country.
Because who can say that we know today much-or enough-of the nature and therapy of phthisis?” -Carlo Forlaniniinserted into the space between the membrane and lung issue (pleural space) and the lung is collapsed by the pressure of the gas. Through collapse of the lung, doctors hoped for closure of tissue cavities by making the organ completely unusable by promoting healing through rest. This practice showed phthisis to nearly cease and patients achieve “favourable results” over the course of 4 or more months (Sakula, 1983, pg 3). As described, before the discovery of the tuberculosis bacterium and therefore antibiotics to fight this disease, extreme measures would be taken to heal patients. Sufferers could face multiple years spent on bed rest in a sanitarium, permanently missing ribs, or even a irreversibly collapsed lung.
Discovery
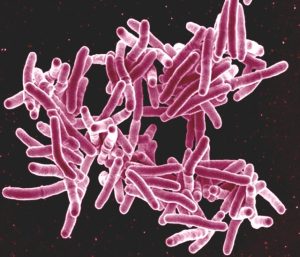
During the era of Tuberculosis Sanitariums, Robert Koch made two major discoveries that affected the course of terror of the tuberculosis outbreak on society: the cause and the detector. In 1882, Koch discovered the etiologic agent of tuberculosis: Mycobacterium tuberculosis. Koch discovered and described the agent as an “infectious disease beyond doubt…” (Kaufmann, 2005, p.1). He concluded that TB was caused by a bacterial infection, with specific attention to microbes as the cause. Shortly after the discovery of the microbe, scientist Selman Waksman used Koch’s observations to develop the antibiotic, streptomycin, a close relative of penicillin, which was effective against tuberculosis, typhoid fever, cholera, bubonic plague, tularemia, and urinary tract infections in humans (American Chemical Society National Historic Chemical Landmarks, 2005). As streptomycin was in the early stages of being implemented into treatments, Koch developed the tuberculin skin test for detection of tuberculosis bacteria within patients (Kaufmann, 2005). This test allowed for confirmation that a patient was infected so that Waksman’s antibiotics could be administered. The study of Tuberculosis to find a cure lead to new and significantly less-invasive treatments for Tuberculosis victims. This development in research and creation of first antibiotics by Koch and Waksman paved the foundation for developments in antibiotics for determining etiologic agents of and treating various other microbe-based diseases.
Modern Medicine
The discovery of the tuberculosis bacterium as well as the development of streptomycin provided new therapies and treatments to be developed for the welfare of society. By 1940, crude death rates from TB dropped to 42 out of every 100,000 people (Achievements in Public Health, 1900-1999: Control of Infectious Diseases, 1999), dramatically reducing the impact of the infection on society. Today, three main controllers are used to treat, contain and prevent the tuberculosis disease: vaccines, chemotherapy, and antibiotics. Although rarely used, highly susceptible demographics, such as young children living with infected persons, are recommended to be vaccinated against tuberculosis as a precaution, thus decreasing the chance of spread of disease. Vaccines provide protection from the tuberculosis bacteria and allow for those who may become exposed to have immunity (Children’s Hospital of Philadelphia, 2020). If the disease has already been contracted, the most effective and commonly used modern cure is

Chemotherapy . The chemicals within chemotherapy are used to treat lung lesions within infected persons, proving dramatically more effective than thoracoplasty or artificial pneumothorax, and lacks overtly invasive treatment. In the 1970s, chemotherapy drugs isoniazid, rifampin, and pyrazinamide were discovered to substantially cut down the duration of tuberculosis therapy to as little as 6 months. Chemotherapy for tuberculosis is administered in intervals, 2-3 times weekly and can cure far-advanced tuberculosis in approximately 6 and a half months (Iseman, 2002). Because of modern-age treatments and precautionary methods, tuberculosis has dramatically decreased among society. However, following the beginning of the HIV epidemic, tuberculosis made its return within the weakened immune systems of AIDS patients. But since 1993, through the use of additional antibiotics and anti-infectives as treatments in AIDS survivors, the number of cases have been decreasing steadily (Children’s Hospital of Philadelphia, 2020). These new-age treatments of tuberculosis have improved life-expectancy and outlook for victims, and also prevented further infection throughout society.
Looking Forward
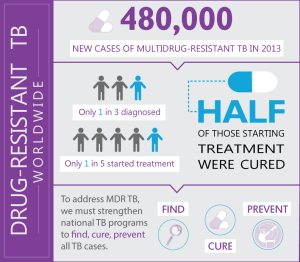
Although TB treatment has come a long way since ribs were removed and lungs deflated, the fight against the illness is yet to be won. However, innovation within science and technology to combat tuberculosis has spurred the field of medicine to improve the course of public health further into the future. Antibiotics were introduced thanks to the works of Waksman and the disease targeted by Koch, but what is yet to be overcome is the challenge of Tuberculosis drug resistance. Because of overuse of antibiotics causing mutations within various bacterias, innovation surrounding Tuberculosis will be continuous, compounding on the scientific advancements already made in combat. While Tuberculosis is not projected to be eliminated in this century (Children’s Hospital of Philadelphia, 2020), further innovation propelled by this daunting challenge for the benefit of mankind will hopefully yield progress to the point that TB no longer exists in the United States. Tuberculosis has led to cures of other infectious diseases, and has overall helped to improve the health of society through science.
Florence Sabin
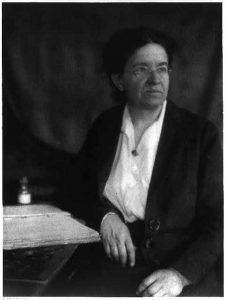
Tuberculosis was more than just a disease to Florence Sabin, it was a gateway. The disease gave this female scientist and researcher a pathway to succeed. The life of Florence Sabin was not only one filled with knowledge and discoveries, it was filled with hope and motivation for other females as they gained confidence in the field of science. The work of Florence Sabin was crucial in research and additional discoveries made about tuberculosis, leaving a lasting impact on females in science.
Florence Sabin was born in Central City, Colorado, in 1871 (Wooley, 2005). She attended the all-women Smith College Northampton, Massachusetts. In 1896, she became one of 14 women in a class of 45 to attend Johns Hopkins Medical School, which had just been built thanks to a group of women who managed to raise enough funding (McGraw, 2018). Sabin was very successful in college, and by 1917, she became the first woman to earn a full professorship at Hopkins’ medical school. In the fall of 1925, Sabin left Hopkins to become a research scientist at The Rockefeller Institute, now known as Rockefeller University (McGraw, 2018).
When she began her research involving tuberculosis, there were already vaccines and research being done about various diseases, except for tuberculosis which affected “80-90 percent of Americans” (McGraw, 2018). Sabin faced many challenges being a woman in science and she moved around many different times to find a position where she felt she could confidently research and be respected in her field as a female (National Institutes of Health, 2005). Susan Speaker, a historian at the National Library of Medicine who has written about Sabin for an NIH online series states that “Sabin’s work furthered knowledge of how TB interacts with elements of the immune system, and why the immune system can’t always defeat it … While it didn’t result in a cure, Sabin’s work significantly advanced knowledge of both tuberculosis and the immune system” (McGraw, 2018).
During this time period, and still today, the voices of females in STEM careers are few. There are gender-barriers set up by society that cause women to feel limited, and inferior to men in this field. Sabin believed, as she wrote in a letter, that it was “better for all women to remove restrictions that are artificial and to permit women to find the level of their own abilities.” (McGraw, 2018). Sabin worked not only to advance the field of science and research, but also to motivate and lead other females to do the same. Sabin later joined a group that was working to build a women’s hospital in New York, which would give women in medicine jobs, but also provide good health care to those who couldn’t always pay (McGraw, 2018).
The question of why there are so few female voices in the field of science is hard to answer. Compared to men, there are few women pursuing a degree in STEM, and this is mainly due to the stigma that society has created. Society has made it clear in various ways that it is better for men to be the ones holding careers in fields such as science and engineering, but the reasons behind that logic are not practical. According to the National Science Foundation, “only 27% of all employees in science and engineering occupations are women” (Fouad et al. 2010). Despite recent movements and advancements in science, women are still facing the consequences of “gender barriers to entry and success of scientific careers” (Etzkowitz et al. 2000).
The problem of gender barriers and stigmas about women in science is not something that should be overlooked. Gender barriers are evident in many areas of society, but especially in STEM careers. It is vital to have voices like Florence Sabin to break those barriers and show that there is no true meaning behind the stigmas that society creates. The life and legacy of Florence Sabin serves as an example of how much of an impact even just one individual can have on not only research and science itself, but also those involved.
A Teen’s fight against tuberculosis

Melissa Sanchez, a healthy teenager living in Lima, Peru, developed extensively drug-resistant tuberculosis at the young age of 17. In June of 2013 Melissa was lying in bed at the hospital while the doctors explained to her why her lungs were strained and why she was constantly coughing blood. “You have tuberculosis” were the words that changed Melissa’s life forever (Sanchez, 2014).
In the summer of 2013, Melissa’s family had a distant relative of her mother’s staying in their home; they ate lunch and breakfast together every day while he was in town. One day her mom was talking with him, and they found out he had an illness; just less than one short month later, Melissa began to feel sick. She had all the symptoms of a cold, so her mom bought her cold medicine from the pharmacy. However, her condition only continued to worsen.
Once Melissa and her mother realized what was happening wasn’t normal, her mother took her to the health center where they gave her a series of exams and chest X-rays. The clinicians in charge, seeing how serious Melissa’s situation was, immediately sent her to the national hospital.
During Melissa’s hospital stay, she learned about tuberculosis and how her and her family could manage it. The doctors finally confirmed what Melissa had feared most. She didn’t have simple TB, but the TB most resistant to drugs: drug-resistant tuberculosis.
Melissa came to accept her illness, and the doctors informed her that there was a cure. It became necessary that Melissa follow a long treatment if she wanted to live. As of 2014, Melissa had completed one year of treatment, receiving fifth-line drugs through a line implanted in her chest beneath the skin. While Melissa receives the treatment in her home alongside her family, she still has to suffer the daily side effects from the medications. Melissa is determined to continue receiving treatments and making others aware of this weary illness.
Chapter Questions
1. Multiple Choice: In what ways did the discovery of the tuberculosis bacteria lead to new scientific advancements?
1) Development of new antibiotics to fight bacteria
2) Improved use of quarantine of tuberculosis patients
3) The formation of antibiotic-resistant bacteria
4) Vaccinations
_______________________________
a) 1&2
b) 3&4
c) 1 & 3
d) all of the above
2. Short answer: In what ways have tuberculosis treatments changed from before the development of streptomycin to now? How are modern treatments better than those before the discoveries by Koch?
3. Multiple Choice-What has been the greatest side effect of antibiotics on society and the path to defeating Tuberculosis?
A) Healthier people with more immunity.
B) Doctors able to use antibiotic research to their benefit.
C) Antibiotic- resistant citizens needing more medication to get better.
References
Achievements in Public Health, 1900-1999: Control of Infectious Diseases. (1999, July 30).
Morbidity and Mortality Weekly Report (MMWR). 48 (29), pg. 621 – 648. Retrieved November 14, 2019, from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4829a1.htm.
American Chemical Society National Historic Chemical Landmarks. (2005). Selman Waksman and Antibiotics – Landmark. Retrieved from https://www.acs.org/content/acs/en/education/whatischemistry/landmarks/selmanwaksman.html.
Castro, K., & Snider, D.E. (1995). Editorial: The Good News and the Bad News about Multidrug-Resistant Tuberculosis. Clinical Infectious Diseases, 21(5), 1265-1266. Retrieved from http://www.jstor.org.libproxy.clemson.edu/stable/4459045
Children’s Hospital of Philadelphia. (2020, May 11). A Look at Each Vaccine: Tuberculosis Vaccine. Vaccine Education Center. https://www.chop.edu/centers-programs/vaccine-education-center/vaccine-details/tuberculosis-vaccine.
Etzkowitz, Kemelgor, C., & Uzzi, B. (2000). Athena Unbound : The Advancement of Women in Science and Technology. Cambridge University Press.
Fouad, N., Singh, R., Wan,M., (2017). Women’s Reasons for Leaving the Engineering Field. Frontiers in Psychology. https://www.researchgate.net/publication/318260107_Women%27s_Reasons_for_Leaving_the_Engineering_Field
Hurt, R. (2004). Tuberculosis sanatorium regimen in the 1940s: a patient’s personal diary. Journal of the Royal Society of Medicine, 97(7), 350–353. doi:10.1258/jrsm.97.7.350. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1079536/.
Iseman, M.D. (2002). Tuberculosis Therapy: past, present, future. European Respiratory Journal, 10(36), 87s-94s. DOI: 10.1183/09031936.02.00309102
Kauffman, S. (2005). 100th Anniversary of Robert Koch’s Nobel Prize for the discovery of the tubercle bacillus. Trends In Microbiology, 13(10), 469-475. doi:10.1016/j.tim.2005.08.003
McGraw, E. (2018, July 6). Florence Sabin pioneered her way in medical science, then made sure other women could do the same. Smithsonian.com. https://www.smithsonianmag.com/science-nature/medical-pioneer-who-pushed-boundaries-science-and-feminism-180969555/
National Institutes of Health. (2015, June 3). Changing the face of Medicine | Florence Rena Sabin. U.S. National Library of Medicine. https://cfmedicine.nlm.nih.gov/physicians/biography_283.html.
Sakula, A. (1983). Carlo Forlanini, inventor of artificial pneumothorax for treatment of pulmonary tuberculosis. Thorax, 38(5), 326–332. doi: 10.1136/thx.38.5.326
Sanchez, M. (2014, August 20). ‘You Have TB’: Melissa Sanchez’s story. Partners In Health. Retrieved September 26, 2021, from https://www.pih.org/article/you-have-tb-Melissa-Sanchez-story.
Sellors, T. H. (1947). The Results of Thoracoplasty in Pulmonary Tuberculosis. Thorax, 2(4), 216–223. doi: 10.1136/thx.2.4.216
University of Virginia Historical Collections at the Claude Moore Health Sciences Library. (2007) Every Breath You Take: Tuberculosis Treatments. http://exhibits.hsl.virginia.edu/breath/desperate-search/.
Wooley, C. F. (2005). Florence Rena Sabin (1871-1953), William Osler (1849-1919) and tuberculosis. Journal of Medical Biography, 13(3), 162-9. http://libproxy.clemson.edu/login?url=https://www-proquest-com.libproxy.clemson.edu/scholarly-journals/florence-rena-sabin-1871-1953-william-osl er-1849/docview/210361684/se-2?accountid=6167
images
“Florence R. Sabin” by Ulmann, Doris
“Robert Koch” by Unknown is in the Public Domain
” Tuberculosis hospital and sanatorium construction” by Carrington, Thomas Spees National Association for the Study and Prevention of Tuberculosis (U.S.) is licensed under CC BY-NC-SA 4.0
“TB poster” by Rensselaer County Tuberculosis Association. is licensed under CC BY-NC-SA 4.0
“Mycobacterium tuberculosis Bacteria, the Cause of TB” by NIAID is licensed under CC BY-NC-SA 4.0
“Infographic: Drug Resistant TB Worldwide” by CDC is licensed under CC BY-NC-SA 4.0
“OraQuick HIV test” by Marcello Casal is licensed under CC BY-NC-SA 4.0
“You Have TB” by Raul Silverio Carbajal

