Health and Medicine
103 Personalized Medicine
Sofia Jones; Anna Holstein; and Paige Richardson
Introduction
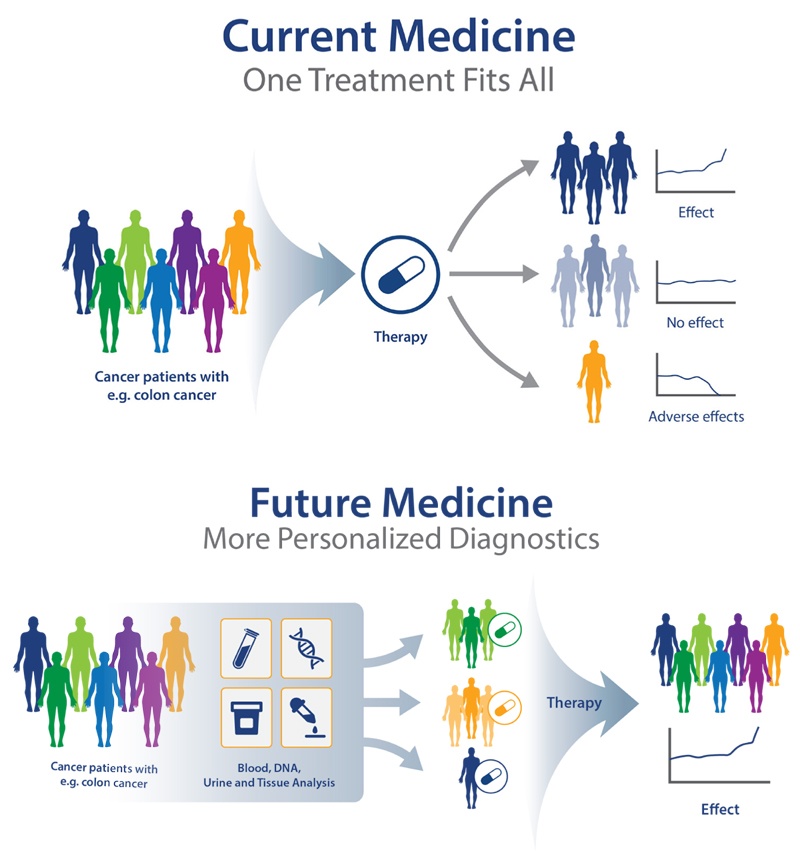 Prescription medication allows for intender patients to treat a specific medical diagnosis, but what if the medicine was engineered for the individual? Personalized medicine is the process of using one’s own genes to diagnose, treat, and prevent diseases, which can ensure better patient care, early treatments and diagnosis, and higher safety margins than current prescription processes. The idea of Personalized Medicine, sometimes called precision medicine, originated in 1999 after publishing “New Era of Personalized Medicine: Targeting Drugs for Each Unique Genetic Profile” in The Wall Street Journal. For the first time, this article revealed the lack of efficiency in current pharmacotherapy:
Prescription medication allows for intender patients to treat a specific medical diagnosis, but what if the medicine was engineered for the individual? Personalized medicine is the process of using one’s own genes to diagnose, treat, and prevent diseases, which can ensure better patient care, early treatments and diagnosis, and higher safety margins than current prescription processes. The idea of Personalized Medicine, sometimes called precision medicine, originated in 1999 after publishing “New Era of Personalized Medicine: Targeting Drugs for Each Unique Genetic Profile” in The Wall Street Journal. For the first time, this article revealed the lack of efficiency in current pharmacotherapy:
“Langreth and Waldholz contained several of the arguments for individualizing pharmacotherapy, as we know them, from the past 20 years of discussions. They stated that the current pharmacotherapy was a ‘one‐size‐fits‐all’ approach in which even the best drugs work in only 50%–70% of the patients” (Jørgensen, 2019).
This concept originates from the idea that diseases along with people are both heterogeneous, therefore medication would be most effective when tailored to different genes, environments, and lifestyles. Although the term wasn’t defined till 1999, the process of combining drugs and diagnosis was first done nearly 2 decades earlier when the selective estrogen receptor modulator tamoxifen was developed for the treatment of breast cancer. Since then, there has been an increase in the molecular understanding of the mechanism of drugs, effectively expanding the concept and practice of using personalized medicine.
Tissue Engineering
Tissue engineering, derived from the field of biomaterials engineering, consists of the artificial development of cells, skin, tissue, or even full organs, typically for medical or research purposes. Although tissue engineering is still being developed and perfected, it has played an important role in patient treatment. One current method being used within tissue engineering is the practice of 3D bioprinting. A research team from Tel Aviv University was able to 3D-print a functioning glioblastoma surrounded by brain tissue and functioning blood vessels. The team used biological samples from patients in order to conduct genetic sequencing of the cancer cells, which replicated the specific growth rate and behavior of each tumor. Professor Ronit Satchi-Fainaro, lead researcher, states, “Cancer, like all tissues, behaves very differently in a petri dish or test tube than it does in the human body. Approximately 90% of all experimental drugs fail in clinical trials because the success achieved in the lab is not reproduced in patients” (Tel Aviv University, 2021). This achievement is a gateway for personalized medicine as different medications in multiple combinations can be tested on hundreds of bioprinted tumors to discover the optimal treatment for the specific tumor. Tissue engineering has also been involved in projects regarding ovarian cancer and even spinal cord injuries, ultimately aiming to create functioning 3D-printed organs capable of being used for transplants.
treatment of psychiatric disorders
So far, personalized medicine has been most commonly used for cancer treatments and research, but what about the disease that affects over 50% of the human population? Mental illness and psychiatric disorders affect nearly 1 in 4 people worldwide, so finding more treatments for these patients is a primary goal for many researchers. Being able to use personalized medicine for the treatment of psychiatric disorders would open the door to accurate diagnoses, efficient responses and treatments, and the ability to predict a patient’s susceptibility to these illnesses. So far, there have been studies conducted on Major Depressive Disorder (MDD), Bipolar Disorder (BD), Schizophrenia (SZ), and more. The most studied drug-metabolizing enzyme in these studies is the cytochrome P450 enzyme. This enzyme is expressed predominantly in the liver but is also found in many extra-hepatic locations, including the brain. It is responsible for nearly 50% of the most commonly prescribed psychotropics, with evidence showing its involvement in the biosynthesis of dopamine. Researchers have pinpointed the use of this enzyme for future use, but it will take time before real implementation can occur. In the future, researchers hope to expand genomic techniques and testing protocols and be able to use a wider variety of substrates. Neuroimaging genomics also shows promise in personalized medicine and psychiatry, allowing the conduction of experiments that relate genetic change to outcomes of tests on brain function (Ozomaro et al., 2013). While there is a lot of promise for the future in personalized medicine, there are issues that arise with this treatment research. Most drugs currently used today are applicable to countless diseases and can be used for almost all patients. Since this type of treatment is specific to the patient and their disease, it is extremely costly and inefficient as each patient would need personalized treatment. Another primary concern is scientific adequacy, as there are so many mental illnesses; therefore, it would be difficult to target each specific condition for individual patients (Evers, 2022). Overall, researchers have proven that there is promise with personalized medicine in treatment of psychiatric disorders, however, there are many limitations and issues that must be addressed before implementation into routine treatment.
Genetic Modification
Genetic modification and gene therapy are relatively new ideas in the field of biomedical engineering. Initially introduced in the 1960s, genetic engineering has been a rapidly evolving field used in many different medical applications, including cancer treatments and genetic diseases. Up to 2024, over 1900 clinical trials have been done related to genetic modification, which is leading the way for future innovation within this area. This type of engineering is specifically done to either introduce or splice out specific genetic sequences that code for a certain protein. The introduction of a genetic code would mean this sequence could deactivate, block, or inhibit the growth or development of a tumor or a genetic disease from its active state. This process can be done to an embryo prior to implantation into the mother (Tamura 2020).
Ethical concerns of genetic modification: Embryonic Development
Ethical concerns have come to light with this new technology, but it is also good that comes from it when it is used as intended. The most dominant advantage of this technology is catching genetic diseases in embryonic development and inactivating them or splicing the sequences that code for the disease out of the embryo in order to take the disease away from the child before they are born. This process corrects genetic mutations that are usually inherited from one of the parents. The benefit of knowing that the parents have a hereditary disease that may get passed along to their child would be that there is now a possibility of getting rid of that mutation entirely. Having the ability to intervene in a child’s development before birth allows for hereditary diseases to be stopped in the bloodline permanently (Peddi 2022).
Personalized medicine and genetic engineering have tremendous potential in today’s society but pose many risks. Exploitation and abuse of this newfound power in technology are some of these risks. Being able to draw the line between ethical and unethical is an important step to take when it comes to this type of innovative medicine. Genetic modification could help thousands of people, but if technology could also be used to create a perfect society, only a certain group within the population would have access to it. These two sides could see a compromise if the technology is solely used for medicine and treating diseases. The manipulation of the natural event that is birth is where a lot of people cross the line, but also where a lot of the population is intrigued and wants to know more about it. Both sides have research and scholars who are backing up either side. Neither side is wrong, but they would be able to come to a compromise that would just be a less extreme version of genetic engineering. The study of genes and the ability to modify them could happen if they were spread out amongst numerous companies and doctors in order to spread the power (Peddi 2022).
Four ethical concerns circulate around gene therapy and genetic modification used as a treatment. Dehumanization, privacy and discrimination, safety, and equal access are the main controversies surrounding genetic modification in embryonic development. The main ethical concern comes into dehumanization and the effects it has on equal access and society as a whole.
Dehumanization is defined as the act of depriving patients of basic human qualities and rights. Looking at this controversy in the context of genetic modification in embryonic development, there is a great possibility for the abuse of this technology in the future of medicine. This encompasses the ability of parents and physicians to “pick” traits for their children (Ma 2017). Thinking about how gene therapy can be used as a tool to mutate genes that are coding for diseases, the same ideology is applied to traits that parents specifically want their children to have. The concern stems from the disruption of basic human nature. The overarching end worry is a “perfect” society being created based on the biased views of people with access to this technology and people with power over society. Traits ranging from gender to enhancing memory and cognition are able to be altered using genetic modification (Christoff 2014).
Impact on society
Personalized medicine tackles a big discrepancy between the medical field and gender issues. While gender is a more fluid term regarding personal identity, it is important to keep in mind the biological differences between the female and male sexes and the impact that they can have on medication. Due to the concern that hormone variability may impact results, researchers often left women out of research studies. Until 2016, this was also found when testing on animals, as it was easier and cheaper to test on one set, typically being male. Nicole Woitoich, associate director of the Women’s Health Research Institute at Northwestern University Feinberg School of Medicine, has noted that sex influences health and treatment; however, many researchers do not look at their results by sex, making it impossible to test which drugs may impact each differently. In a recent study regarding brain tumors, Wotoich also noted how, when analyzing the data by sex, it was found that they responded differently to treatments (Gordon, 2020). This is important as women are often left with undiagnosed diseases due to having different symptoms than men. With personalized medicine, looking at an individual’s gene structure would completely eliminate the issue, as all treatments would be completely tailored for the individual.
future directions: implications for public health
While the very nature of personalized medicine implies individual patient focus, its influence is beginning to expand into the realm of public health. By analyzing genetic trends, environmental exposures, and lifestyle factors across large populations, public health officials can now design targeted interventions that address the specific needs of different communities.
The integration of personalized medicine into public health initiatives could help address longstanding health disparities. For example, certain genetic predispositions to diseases like hypertension or diabetes are more prevalent in specific populations with correlating demographics. By clearly identifying these patterns, healthcare systems can develop prevention programs accordingly. From there, personalized medicine tactics can be prioritized and implemented. However, this approach raises concerns about reinforcing racial or socioeconomic stereotypes if not handled carefully.
Another important consideration is the ethical management of population-level health data. Public health efforts that rely on personalized medicine require access to databases containing sensitive genetic and medical information. Balancing the need for large-scale data analysis concerning individual privacy will require new forms of regulation, community consent, and transparency. Public trust in healthcare institutions may hinge on how these issues are navigated as personalized public health programs expand.
Ultimately, personalized medicine’s influence on public health challenges the traditional boundary between individualized care and collective wellbeing, blending technological innovation with social responsibility. As personalized approaches become more common, future public health policies must integrate scientific advancements with ethical considerations, ensuring that technology serves individuals and the broader societal good.
Conclusion
Personalized medicine is a moderately new practice that holds a lot of potential for the future of medication, providing access to treatments that are more effective than ever before. Personalized medicine is a gateway for rapidly functioning treatments, cutting down costs and avoiding the “trial and error” stage of prescribed medications that will continue to develop along with technology such as tissue engineering.
Chapter Questions
- Short Answer: Where and when was the term “personalized medicine” first used?
- True or False: Prescription medication is the most effective way to treat diseases for all kinds of patients.
- Short Answer: Why might researchers need to consider sex when analyzing data?
- Short Answer: Why is it difficult to make advancements in personalized medicine related to psychiatric disorders?
- Short Answer: What are the limitations of using personalized medicine as a treatment instead of common antibiotics or drugs?
References
Christoff K. (2014). Dehumanization in organizational settings: some scientific and ethical considerations. Frontiers in human neuroscience, 8, 748. https://doi.org/10.3389/fnhum.2014.00748
Evers, K. (2022). Personalized medicine in psychiatry: ethical challenges and opportunities. Dialogues in clinical neuroscience. https://www.tandfonline.com/doi/full/10.31887/DCNS.2009.11.4/kevers
Gordon, S. (2020, June 10). Women still left out of much medical research. Medical Xpress
-medical research advances and health news. Retrieved October 23, 2021, from
https://medicalxpress.com/news/2020-06-women-left-medical.html.
Jørgensen J. T. (2019). Twenty Years with Personalized Medicine: Past, Present, and
Future of Individualized Pharmacotherapy. The oncologist, 24(7), e432–e440.
Ma, H., Marti-Gutierrez, N., Park, S. W., Wu, J., Lee, Y., Suzuki, K., Koski, A., Ji, D., Hayama, T., Ahmed, R., Darby, H., Van Dyken, C., Li, Y., Kang, E., Park, A. R., Kim, D., Kim, S. T., Gong, J., Gu, Y., Xu, X., … Mitalipov, S. (2017). Correction of a pathogenic gene mutation in human embryos. Nature, 548(7668), 413–419. https://doi.org/10.1038/nature23305
Ozomaro, U., Wahlestedt, C., & Nemeroff, C. B. (2013). Personalized medicine in psychiatry: problems and promises. BMC medicine, 11(1), 1-35. https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-11-132
Peddi, N. C., Marasandra Ramesh, H., Gude, S. S., Gude, S. S., & Vuppalapati, S. (2022). Intrauterine Fetal Gene Therapy: Is That the Future and Is That Future Now?. Cureus, 14(2), e22521. https://doi.org/10.7759/cureus.22521
Tamura, R., & Toda, M. (2020). Historic Overview of Genetic Engineering Technologies for Human Gene Therapy. Neurologia medico-chirurgica, 60(10), 483–491. https://doi.org/10.2176/nmc.ra.2020-0049
Tel Aviv University. (2021, November 24). 3D printing takes on Brain Cancer. Tel Aviv
University. Retrieved December 3, 2021, from https://english.tau.ac.il/news/3d_printing_brain_cancer.
Khoury, M. J., Iademarco, M. F., & Riley, W. T. (2016). Precision public health for the era of precision medicine. American Journal of Preventive Medicine, 50(3), 398–401. https://doi.org/10.1016/j.amepre.2015.08.031
Fullerton, S. M., & Lee, S. S.-J. (2011). Secondary uses and the governance of de-identified data: Lessons from the Human Genome Diversity Panel. BMC Medical Ethics, 12(1), Article 16. https://doi.org/10.1186/1472-6939-12-16
Ashley, E. A. (2016). Towards precision medicine. Nature Reviews Genetics, 17(9), 507–522. https://doi.org/10.1038/nrg.2016.86
Manolio, T. A., Chisholm, R. L., Ozenberger, B., Roden, D. M., Williams, M. S., Wilson, R., Ginsburg, G. S. (2015). Implementing genomic medicine in the clinic: The future is here. Genetics in Medicine, 17(12), 954–964. https://doi.org/10.1038/gim.2015.11
Images and Media
Tel Aviv University (2021). Scientific breakthrough in the battle against cancer: First 3D printing of glioblastoma cancer tumor https://youtu.be/oUjuFyLF5nM
“PDX and Personalized Medicine” by Jody Barbeau PhD is licensed under CC BY 4.0

