Health and Medicine
105 Rheumatoid Arthritis and its Treatments
Taylor Nutzman and Lucas Miller
Introduction
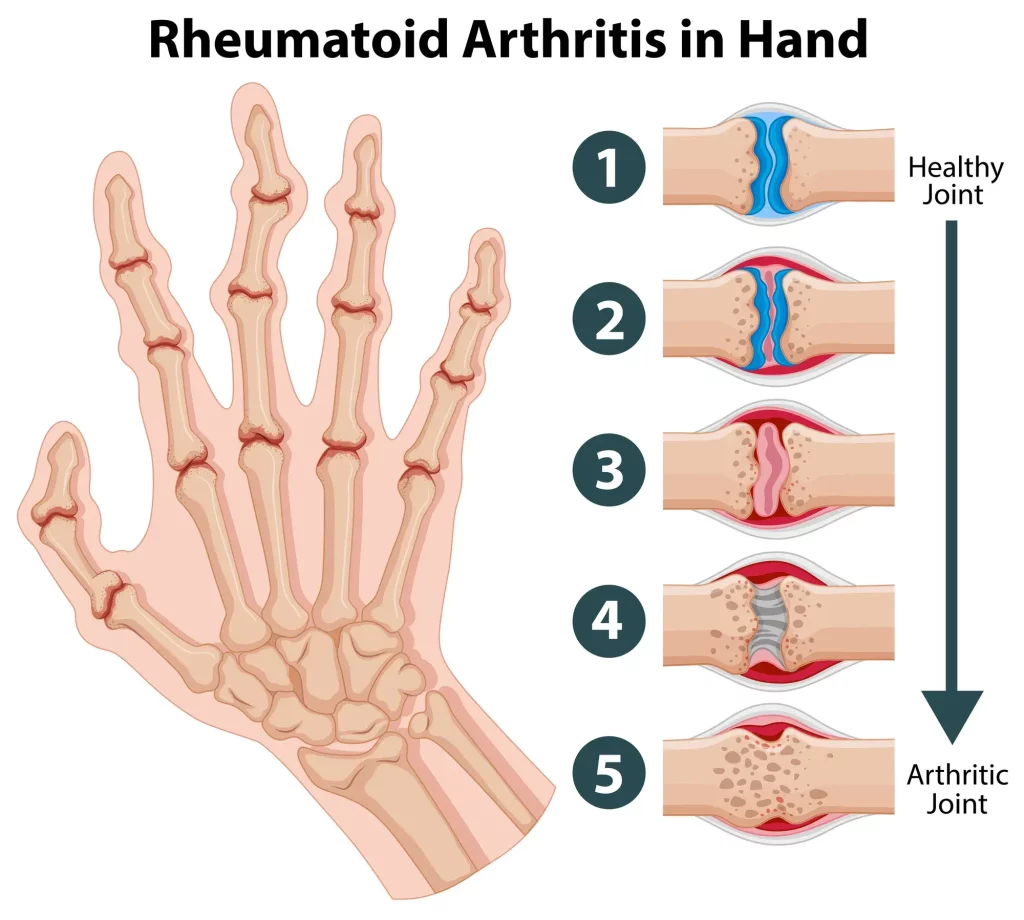
Rheumatoid arthritis is an autoimmune disorder where your immune system attacks the body’s tissues and creates chronic inflammation. This affects the lining of the joints, causing swelling that often leads to bone erosion and joint damage (Mayo Foundation, 2023). Scientists estimate that about 1.5 million people, or roughly 0.6% of the US adult population, have rheumatoid arthritis. This autoimmune disease can occur in all races, ethnic groups, and sexes. However, it is more likely to occur in women than in men (NIH, 2016). Rheumatoid arthritis most commonly develops between the ages of 30 and 60. If the disease affects patients between the ages of 16 and 40, it is considered young-onset rheumatoid arthritis. On the other hand, if symptoms develop after the age of 60, it is considered later-onset rheumatoid arthritis (Rheumatoid Arthritis (RA), 2024). The most common signs and symptoms of rheumatoid arthritis include tender or swollen joints, joint stiffness, fatigue, fever, and loss of appetite. Rheumatoid arthritis typically affects the fingers, hands, wrists, knees, ankles, feet, and toes (Mayo Foundation, 2023). In addition to affecting your joints, it can also impact the skin, eyes, mouth, lungs, and heart. RA is typically diagnosed through physical exams, blood tests, medical imaging techniques, and other diagnostic techniques depending on the patient (Rheumatoid Arthritis (RA), 2024). This chapter discusses rheumatoid arthritis in detail, emphasizing the need for early diagnosis and a comprehensive treatment plan that incorporates pharmacological intervention, lifestyle modifications, and therapies, all of which aim to improve patient quality of life.
Connection to STS
The topic of rheumatoid arthritis connects to science and technology because scientific research plays a crucial role in developing new treatment options and improving patient outcomes. Advances in understanding the underlying mechanisms of the disease have led to the creation of targeted biologic therapies that can better manage symptoms and slow disease progression. Ongoing studies continue to explore potential treatments, offering hope for more effective and personalized care in the future. This is connected to society because improved treatment options can significantly enhance the quality of life for individuals living with rheumatoid arthritis. As patients experience fewer symptoms and more manageable disease progression, they can maintain their independence and productivity, which can reduce healthcare costs and lessen the economic burden on families and communities. Additionally, these advancements contribute to increased awareness and understanding of the condition, fostering a more supportive and inclusive society.
Rheumatoid arthritis research also demonstrates the important role that government and institutional support play in developing treatment strategies and disseminating public health information. Agencies like the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS, 2016) fund and publish evidence-based resources to improve early diagnosis, educate the public, and guide clinical decision-making (NIAMS, 2016). These efforts reflect how scientific knowledge is shaped and shared within society and demonstrate the value of institutional science in bridging healthcare gaps and improving population-level outcomes.
Treatments for Rheumatoid arthritis
Historically, treatment for rheumatoid arthritis was limited to managing symptoms with physical therapy and non-specific pain relief. The development of corticosteroids revolutionized RA treatment, these drugs offered rapid symptom control and revolutionized patient outcomes. furthermore, both the development of DMARDs in the 1980s and biologic therapies in the 1990s, have significantly improved long-term outcomes for patients, transforming RA from a severely disabling disease to one that can be managed with early therapy (NIAMS, 2016).
There are a variety of different treatment options for Rheumatoid arthritis. These include medications, lifestyle changes, therapies, or even surgery. While there is no known cure for Rheumatoid Arthritis, treatment typically aims to reduce inflammation, manage pain, and slow the progression of the disease. This helps to minimize joint damage and improve physical function and quality of life (Johns Hopkins, 2020). The most common treatment used is medications. The medications can be broken down into three types: non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying anti-rheumatic drugs (DMARDs). Non-steroidal anti-inflammatory drugs (NSAIDs) are known for reducing inflammation, which reduces pain and improves function. Common examples of these are aspirin, ibuprofen, naproxen, and more. High doses of these are typically necessary to decrease inflammation, but once they are taken, they can have an anti-inflammatory effect within hours. Gastrointestinal disturbance is the most common side effect, but it can also impair renal function and increase blood pressure (Johns Hopkins, 2020). Corticosteroids have both anti-inflammatory and immunoregulatory activity. They can provide rapid relief from pain and swelling, making them particularly useful during disease flares or when initiating treatment. They can be given orally, intravenously, intramuscularly, or injected directly into the joint. Some examples are prednisone, methylprednisolone, and Medrol. While corticosteroids can be effective in controlling symptoms, they are typically prescribed at the lowest effective dose (5 to 10 mg daily) for the shortest duration necessary to minimize potential side effects. Side effects of taking these are weight gain, increased fat deposition around the face, redness of the face, increased blood pressure, increased blood sugar, and more (Johns Hopkins, 2020).
In many cases, corticosteroids are used in conjunction with disease-modifying antirheumatic drugs (DMARDs) to enhance overall treatment efficacy and maintain long-term disease control. Disease-modifying antirheumatic drugs (DMARDs) work by modifying the underlying disease process, rather than just treating symptoms, to slow down the progression of RA and prevent joint damage. The two types of DMARDs are traditional (synthetic) and biologic (Johns Hopkins, 2020). Traditional (synthetic) DMARDs have been around for much longer than biologic DMARDs. These include Methotrexate, Sulfasalazine, Hydroxychloroquine, JAK inhibitors, and more. Biologic DMARDs are much newer and were made using biotechnology. They target the specific molecules that cause inflammation in your joints. They are seen as more effective because they attack the cells at a more specific level. Biologics tend to work rapidly, within two to six weeks. These include TNF inhibitors, B-cell inhibitors, T-cell inhibitors, and more (Prasad et al., 2023). DMARDs are typically recommended to older patients before the other medications because they want to target the spots of inflammation as quickly and directly as possible (Pavlov-Dolijanovic et al., 2023). Lifestyle changes that help reduce some of the symptoms of rheumatoid arthritis include diet changes, regular exercise, adequate rest, stress reduction, and more. Therapies that can help manage symptoms include physical therapy, occupational therapy, acupuncture, massage therapy, and more. Surgery is only used to restore function to severely damaged joints. It can also be used if pain isn’t controlled with medication. Typically, these are seen in the form of replacements like a knee or hip replacement (Rheumatoid Arthritis (RA), 2024).
Biologic therapies have significantly advanced the treatment options available for rheumatoid arthritis. These medications are engineered to target specific parts of the immune system that drive inflammation and joint damage. Biologics such as TNF inhibitors, IL-6 receptor blockers, and B-cell or T-cell modulators have demonstrated effectiveness in reducing symptoms and preventing disease progression (Curtis & Singh, 2011). Unlike traditional DMARDs, biologics work more precisely, though they also come with considerations such as higher cost and potential side effects, including increased susceptibility to infection (Curtis & Singh, 2011). Emerging treatment paradigms also explore combination therapies that pair biologics with other DMARDs to enhance effectiveness and minimize disease activity (Curtis & Singh, 2011).
Risk Factors and Complications
Rheumatoid arthritis (RA) is a chronic autoimmune condition that primarily affects the joints and presents several risk factors and potential complications. Women are significantly more likely to develop RA than men, and while it can occur at any age, it is most commonly diagnosed in middle-aged individuals. A family history of the disease also increases the risk, along with lifestyle factors such as smoking and obesity (Mayo Foundation, 2023). Complications of RA can be serious and include a higher likelihood of developing osteoporosis, rheumatoid nodules, and dry eyes and mouth. Additionally, individuals with RA face increased risks for infections, carpal tunnel syndrome, heart problems, lung disease, and lymphoma (Mayo Foundation, 2023). These complications underscore the importance of early diagnosis and effective management of the condition.
In addition to physical complications, rheumatoid arthritis can have significant socio-economic impacts. Research shows that the early years of RA often lead to increased work disability, reduced working hours, and lower overall income, even in patients who begin treatment early (Albers et al., 1999). This impact on employment and productivity highlights the need for timely diagnosis and effective treatment strategies. The financial burden is not only due to medical costs but also the indirect costs associated with lost wages and job limitations (Albers et al., 1999). The chronic pain and functional limitations associated with RA often contribute to depression, anxiety, and decreased quality of life. Understanding these broader consequences of the disease helps emphasize why early management is essential not only for physical health but also for maintaining social and economic stability.
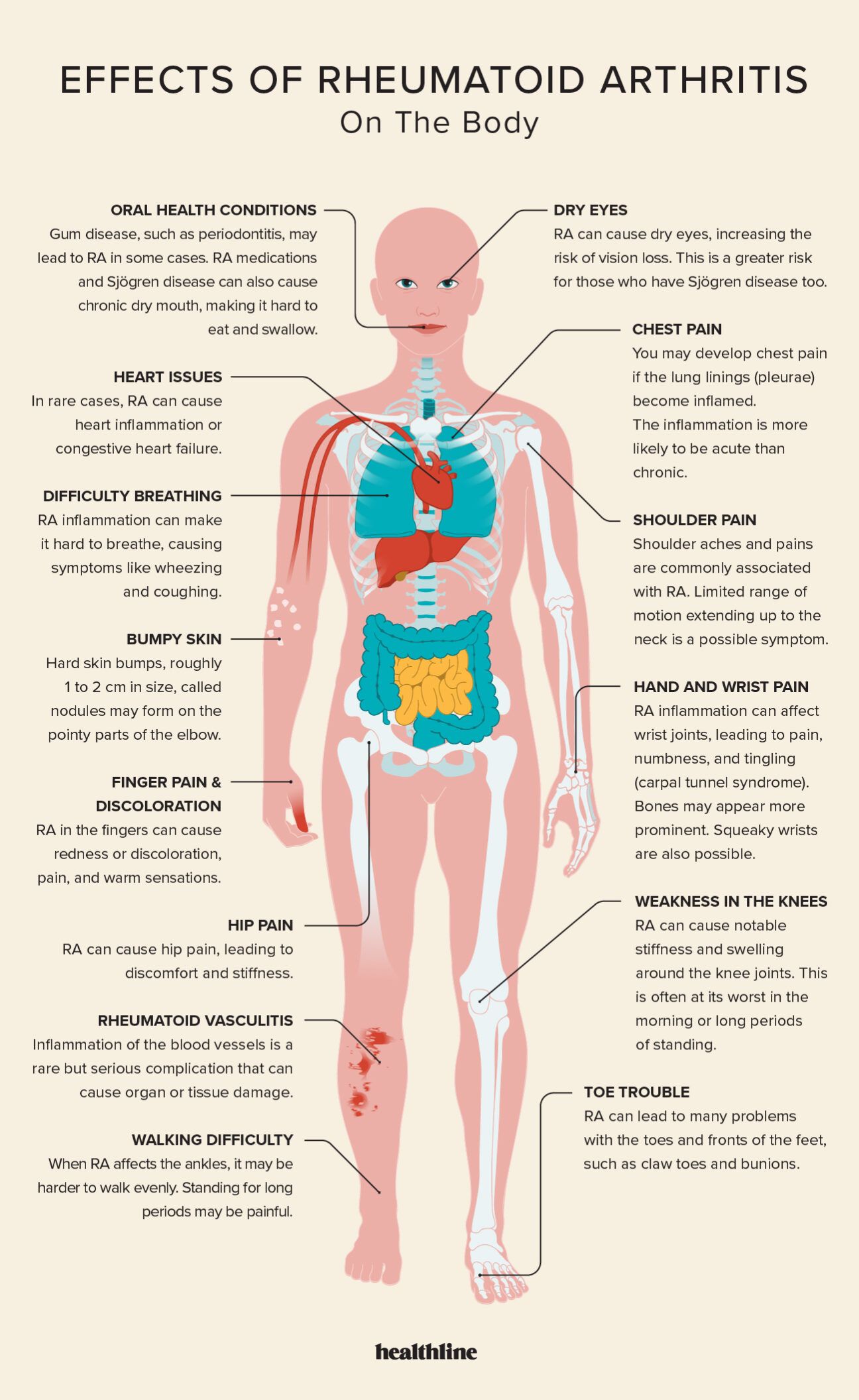
Effects of Rheumatoid Arthritis On The Body
Missing Voices
Unfortunately, medications for this autoimmune disease can be pretty expensive. Even with the help of insurance, patients can spend thousands of dollars annually on the care that they need. This means that some people who would benefit from treatments like these are unable to access them because of the price. This financial burden can lead to feelings of hopelessness and anxiety as patients struggle to manage their health without the necessary medications. The stress of choosing between essential treatments and other basic needs can take a significant emotional toll, leading to a diminished quality of life. For many, the inability to afford proper care not only affects their physical well-being but also weighs heavily on their mental health. A potential solution to the problem could be programs like Remistart that help pay for Remicade treatment. This is a program that you have to apply to and be eligible for; however, if accepted, they will help pay for your treatment. Although not everyone will be treated with Remicade, there are likely other programs out there that could help pay for other treatments. These programs could also be created to help people afford their medications.
Another challenge in managing rheumatoid arthritis is bridging the gap between patient expectations and treatment outcomes. Studies show that both patients and rheumatologists often face difficulties in achieving optimal disease control due to factors such as medication side effects, access to care, and differing perceptions of disease severity (Owensby et al., 2020). Patients may struggle to communicate their symptoms effectively or hesitate to escalate treatment due to concerns about safety or cost, while physicians may prioritize measurable outcomes like lab results or joint swelling (Owensby et al., 2020). These disparities can lead to frustration and reduced treatment satisfaction, making shared decision-making and open communication vital in improving patient care and treatment adherence.
Conclusion
In conclusion, rheumatoid arthritis (RA) presents a complex challenge that significantly impacts the lives of millions worldwide. This autoimmune condition not only causes debilitating joint pain and inflammation but also affects various aspects of physical and emotional well-being. Throughout this chapter, we have explored the multifaceted nature of RA, including its symptoms, diagnosis, and the variety of treatment options available. Current treatment strategies encompass a range of approaches, from pharmacological interventions, such as disease-modifying antirheumatic drugs (DMARDs) and biologics, to physical therapy and lifestyle modifications (Johns Hopkins, 2020). While these treatments can substantially improve the quality of life for many patients, barriers such as high costs, limited access to care, and variability in response to treatment underscore the need for a more equitable healthcare system. Future research in RA is focused on precision medicine approaches, specifically to tailor treatments based on individual patient biomarkers. Advances in gene therapy, microbiome research, and biologic agents could lead to an even more targeted and effective treatment solution, with the goal of achieving sustained remission or even a cure. Ultimately, by recognizing the complexities of rheumatoid arthritis and striving for comprehensive, accessible care, we can work towards improving the lives of individuals impacted by this chronic condition.
Chapter Questions
1.) Short Answer: What joints are commonly affected by rheumatoid arthritis?
2.) True/False: Rheumatoid arthritis is an autoimmune disease.
3.) Short answer: Is rheumatoid arthritis more common in men or women?
4.) True/false: There is a cure for rheumatoid arthritis.
5.) True/False: Exercise is harmful for people with rheumatoid arthritis.
A. RA only affects joints and does not involve other organ systems.
References
Albers, J. M., Kuper, H. H., van Riel, P. L., Prevoo, M. L., van ‘t Hof, M. A., van Gestel, A. M., & Severens, J. L. (1999). Socio-economic consequences of rheumatoid arthritis in the first years of the disease. Rheumatology (Oxford), 38(5), 423–430. https://doi.org/10.1093/rheumatology/38.5.423
Curtis, J. R., & Singh, J. A. (2011). Use of biologics in rheumatoid arthritis: current and emerging paradigms of care. Clinical Therapeutics, 33(6), 679–707. https://doi.org/10.1016/j.clinthera.2011.05.04
Elena Nikiphorou, Hannah Jacklin, Ailsa Bosworth, Clare Jacklin, Patrick Kiely, Disease impact of rheumatoid arthritis in patients not treated with advanced therapies; survey findings from the National Rheumatoid Arthritis Society, Rheumatology Advances in Practice, Volume 5, Issue 1, 2021, rkaa080, https://doi.org/10.1093/rap/rkaa080
Healthline. (2024). Effects of rheumatoid arthritis: Skeletal system, immune, and more. https://www.healthline.com/health/rheumatoid-arthritis/effects-on-body
Mayo Foundation for Medical Education and Research. (2023, January 25). Rheumatoid arthritis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648
National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2016). Rheumatoid Arthritis. Department of Health and Human Services, National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Owensby, J. K., Chen, L., O’Beirne, R., Ruderman, E. M., Harrold, L. R., Melnick, J. A., Safford, M. M., Curtis, J. R., & Danila, M. I. (2020). Patient and rheumatologist perspectives regarding challenges to achieving optimal disease control in rheumatoid arthritis. Arthritis Care & Research, 72(7), 933–941. https://doi.org/10.1002/acr.23907
Pavlov-Dolijanovic S, Bogojevic M, Nozica-Radulovic T, Radunovic G, Mujovic N. Elderly-Onset Rheumatoid Arthritis: Characteristics and Treatment Options. Medicina. 2023; 59(10):1878. https://doi.org/10.3390/medicina59101878
Prasad, P., Verma, S., Surbhi et al. Rheumatoid arthritis: advances in treatment strategies. Mol Cell Biochem 478, 69–88 (2023). https://doi.org/10.1007/s11010-022-04492-3
Rheumatoid arthritis (RA): Causes, symptoms & treatment faqs. Cleveland Clinic. (2024, August 15). https://my.clevelandclinic.org/health/diseases/4924-rheumatoid-arthritis
NIAMS. (2016). Rheumatoid arthritis. Handout on Health. https://permanent.fdlp.gov/gpo72222/Handout%20on%20Health%20%20Rheumatoid%20Arthritis.htm
Rheumatoid arthritis physical therapy in Manhattan & Brooklyn, NYC. Physical Therapists NYC. (2022, December 23). https://www.physicaltherapistsnyc.com/physical-therapy-services/rheumatoid-arthritis/
Rheumatoid arthritis treatment options. Johns Hopkins Arthritis Center. (2020, April 14). https://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-treatment/
AI acknowledgement
This chapter has been authored with the assistance of Microsoft Copilot, an artificial intelligence platform. It was specifically used to help me outline and write small portions of my chapter.

